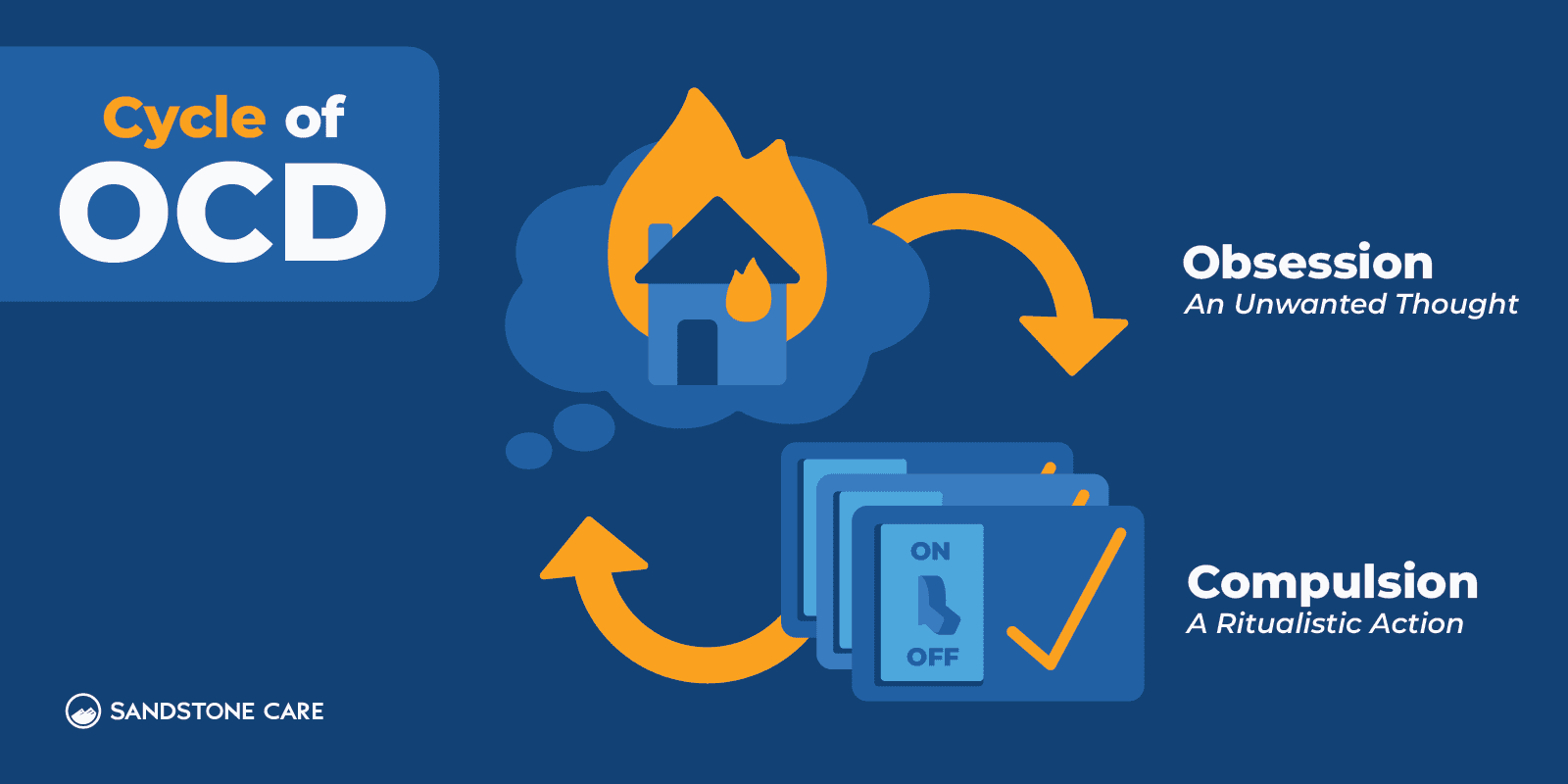
Obsessive-compulsive disorder (OCD) is a chronic, long-lasting disorder that involves uncontrollable, reoccurring thoughts (obsessions) and behaviors (compulsions) that a person feels they need to repeat over and over.
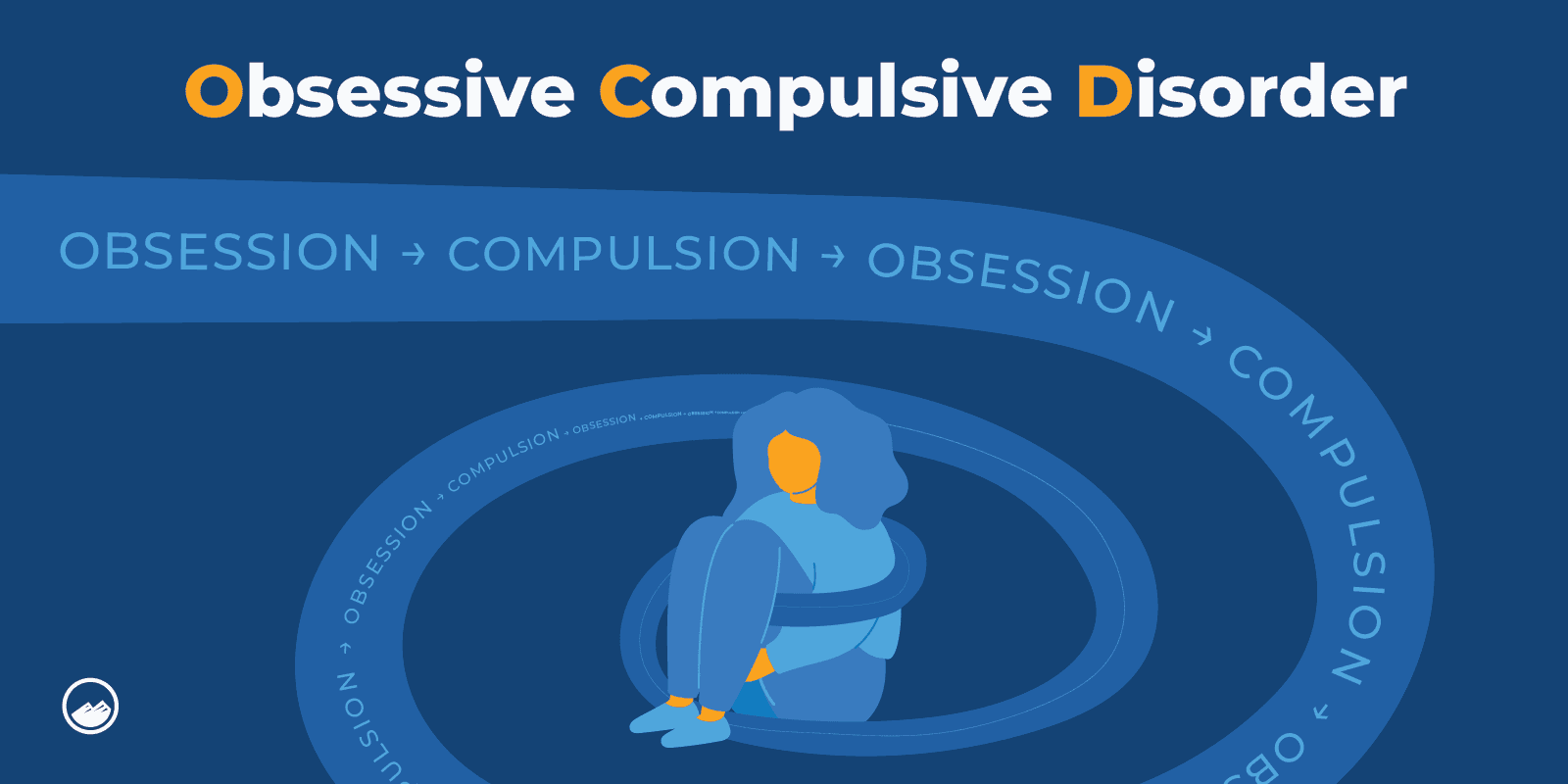
A person with OCD experiences intrusive thoughts that can be distressing and cause discomfort. To manage or reduce this stress, they may engage in compulsions or rituals. These obsessions and compulsions can impact a person’s daily life and cause them significant distress.
OCD is considered a mental health disorder.
Obsessive-compulsive disorder is a common mental illness that has a lifetime prevalence in the United States that ranges from 1.6 percent to 2.3 percent, according to the Substance Abuse and Mental Health Services Administration.
Many people don’t take the time to learn more or understand OCD.
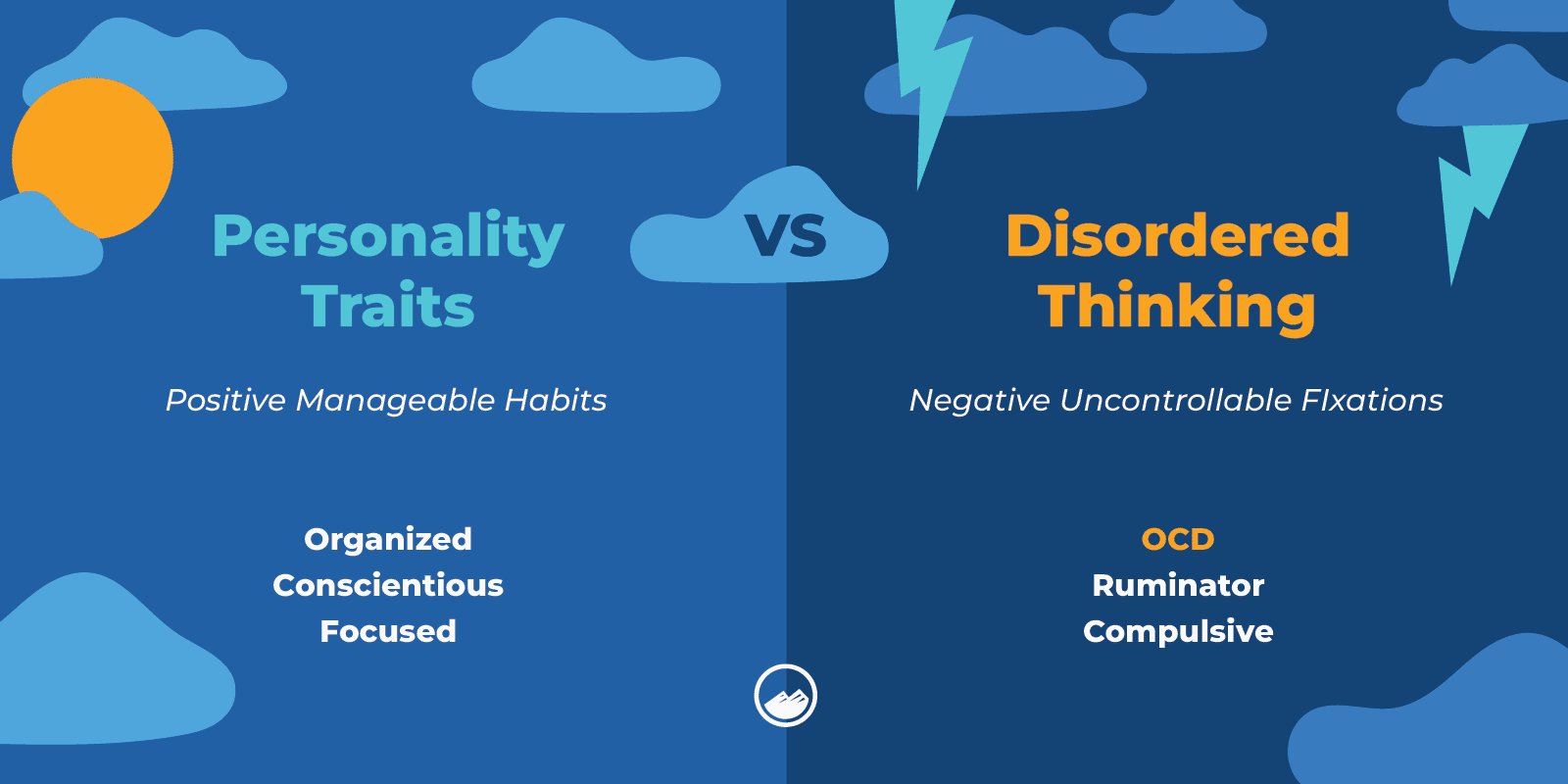
Sometimes people assume that symptoms of OCD are just personality traits and that a person chooses to be a particular way. They may think that the person is making up their symptoms or exaggerating them.
OCD is often portrayed in movies or television by an individual who has extraordinary talents plus the eccentricities of OCD behaviors.
While these portrayals may not mean to romanticize the disorder, they can downplay the negative impact and severity of the disorder by reducing it to comedic quirks or cartoonish displays.
Others may be frightened of or stereotype extreme examples of OCD. For example, people with hoarding disorder are often judged harshly in communities and in the media. This stigma can make people experiencing the same symptoms hesitant to reach out for treatment.
The stigma around OCD can be changed by talking more about it and taking the time to understand others without judgment.
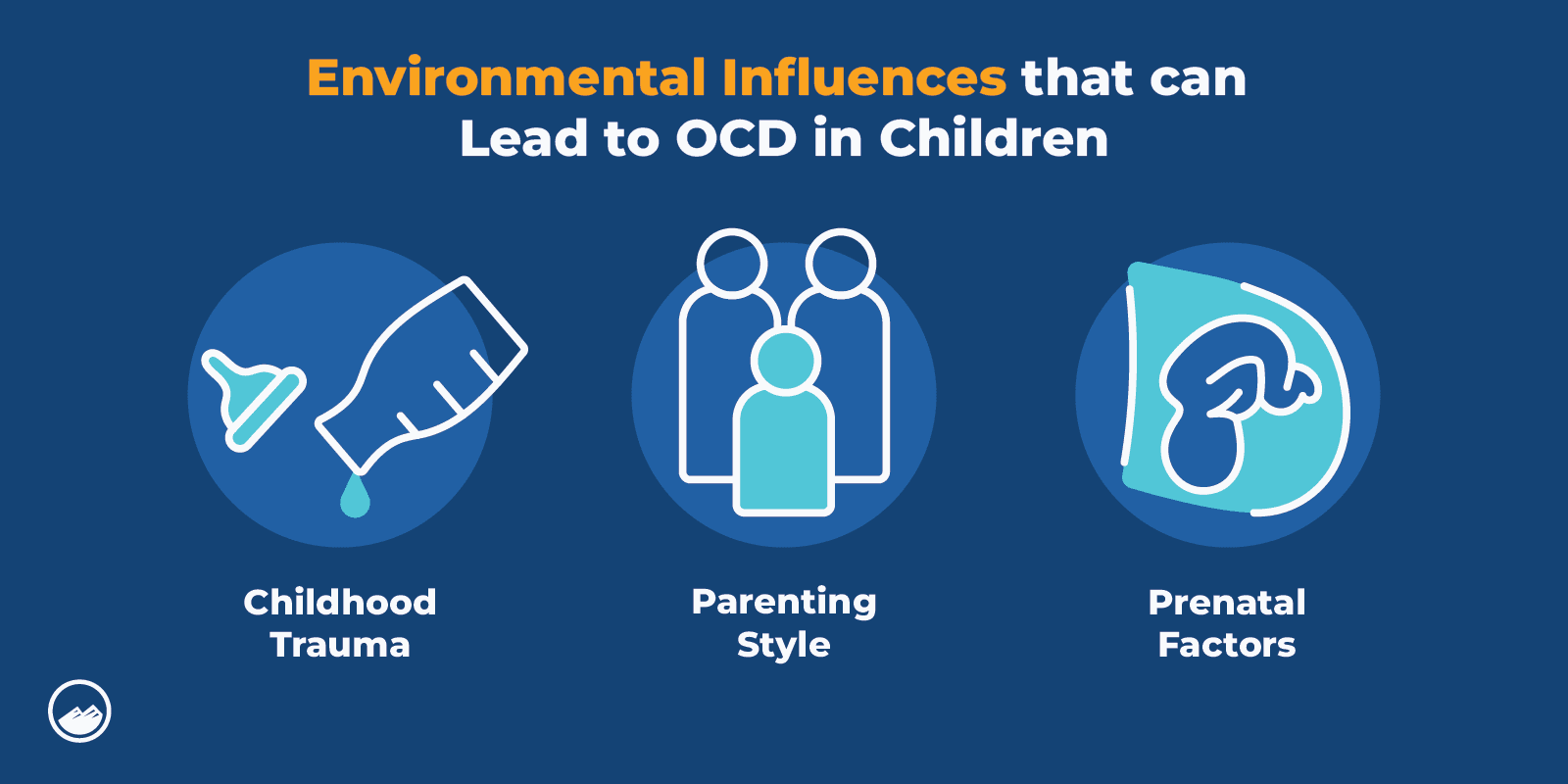
Studies show that OCD can be genetic but may also be environmental or caused by experiences of childhood trauma.
OCD is commonly misdiagnosed as generalized anxiety disorder, which can sometimes be a related disorder.
Other disorders are often linked to OCD and can worsen OCD symptoms. There is a significant amount of research that shows OCD and Bipolar Disorder, or related disorders, to be highly linked to one another.
Depression also shows a high prevalence among those who have been diagnosed with OCD. Those with OCD show a higher likelihood of experiencing dysthymia, a long-term mild form of depression, than the general population.
It is also commonly mistaken for other mental health disorders, such as:
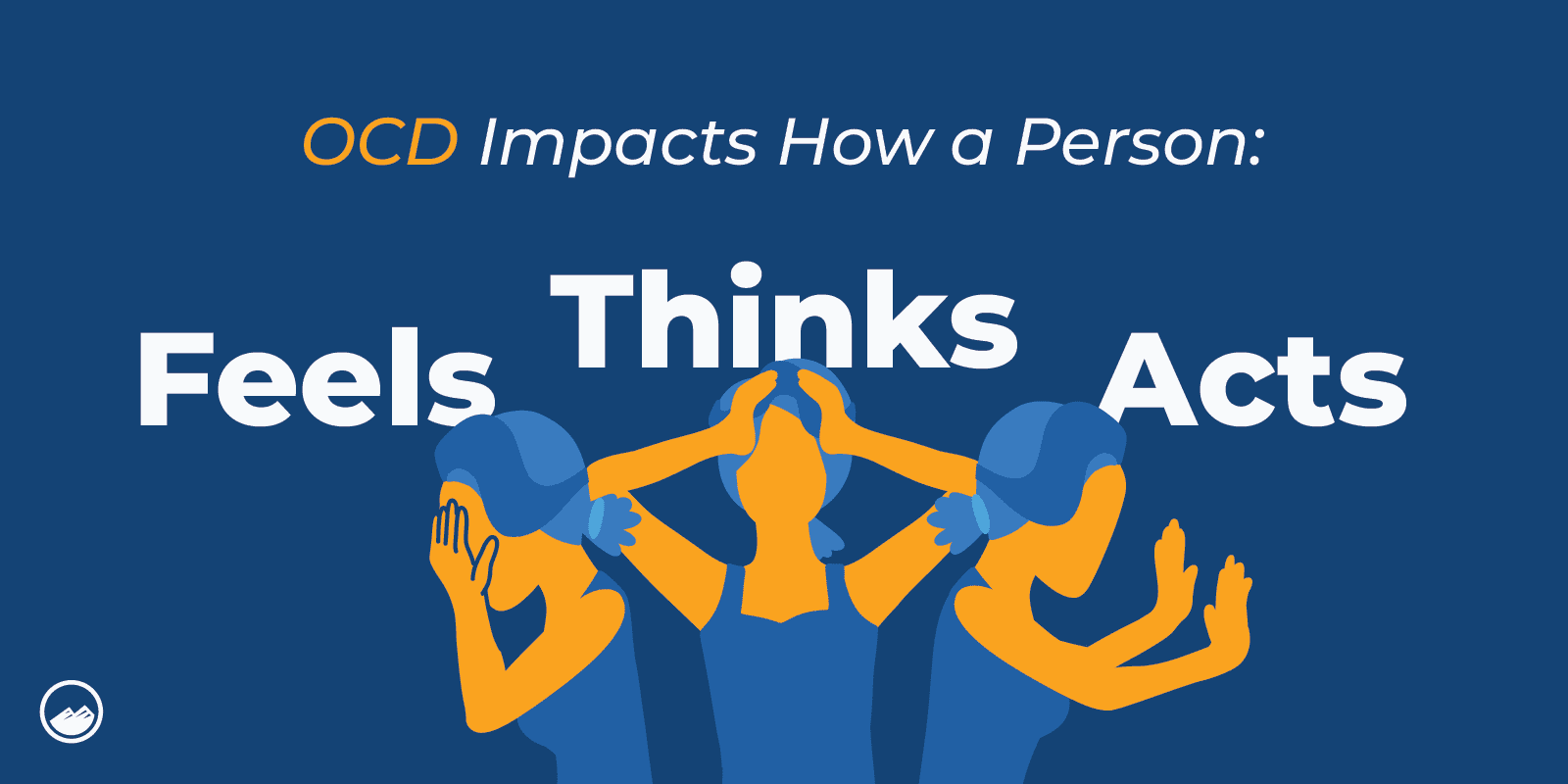
OCD can impact almost every aspect of a person’s daily life.
It can make it difficult to focus and concentrate, creating challenges in places like work or school. Compulsive behaviors and obsessions can also impact a person’s family and social relationships. It can affect how a person views themselves and the world around them.
Managing symptoms in people with OCD without help and support can be very difficult and distressing. This can cause people with OCD to feel lonely and avoid people or specific places.
OCD can impact how a person feels, thinks, and acts in everyday life.
A major misconception about OCD is that it is a personality trait or character flaw. Many people may comment that they have OCD because they prefer things a certain way or like to have things clean and organized.
Dismissive comments like these can hurt individuals who are experiencing the symptoms of OCD and facing challenges. While some common compulsions may look like personality traits, OCD cannot be reduced to a habit or preference.
OCD can come in many forms. There aren’t necessarily defined types of OCD, but there are common symptom categories of OCD.
These can include:
OCD is also related closely to obsessive-compulsive personality disorder (OCPD), which is motivated by a sense of extreme rightness instead of being motivated by fear.
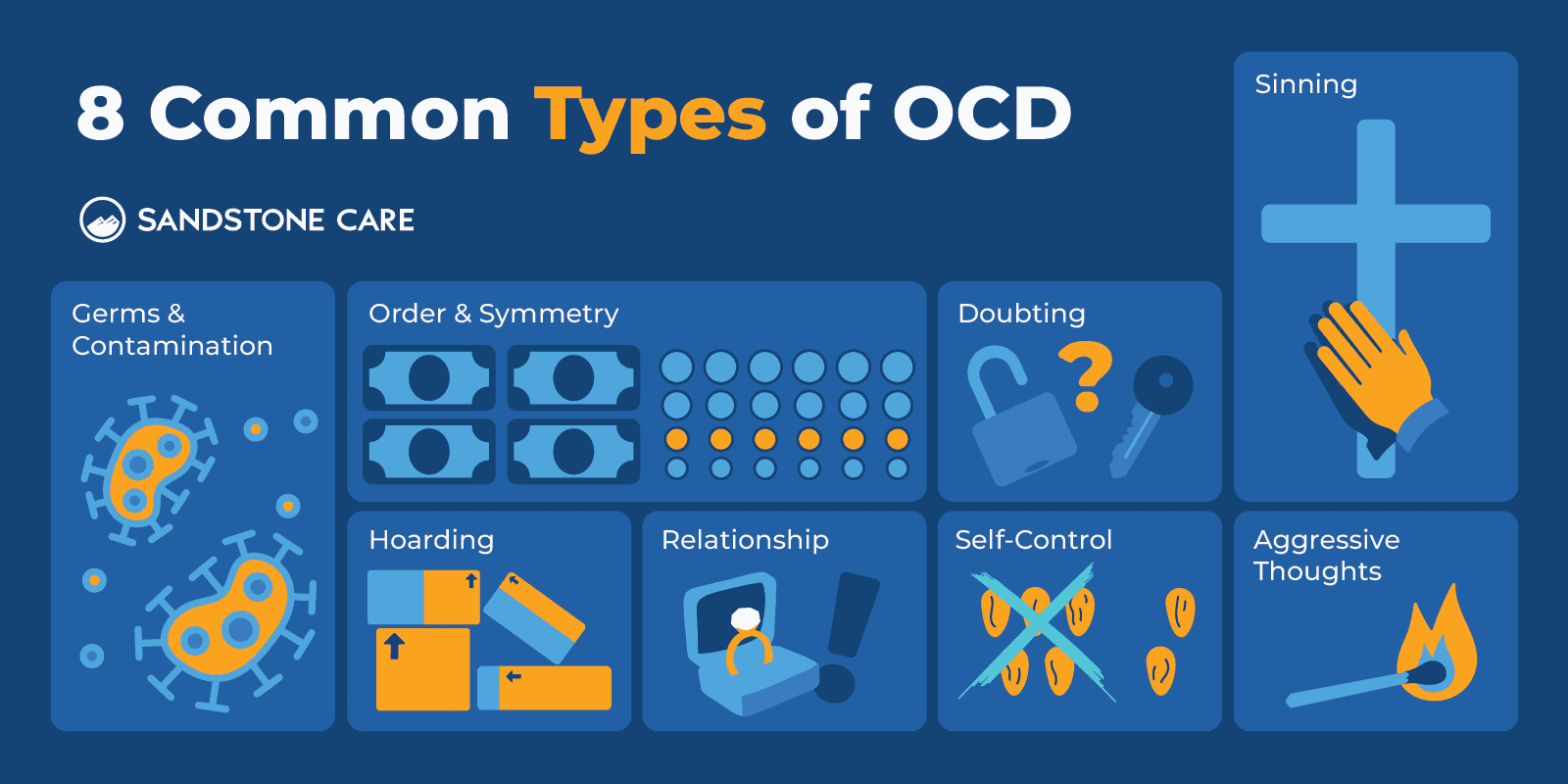
Obsessions and compulsions around contamination and germs are typically the most common type of OCD.
For example, common obsessions around contamination can lead to obsessions like excessive handwashing.
One of the least common types of OCD is harm OCD, where a person experiences intrusive thoughts of harming others or engaging in a violent act. It is important to remember that just because someone struggles with obsessive-compulsive disorder does not mean they are inherently violent or dangerous.
The exact cause of OCD is unknown.
Certain risk factors can include:
The root cause of OCD is unknown but can have much to do with a person’s family history, brain structure and function, and environment.
More specifically, childhood trauma may be linked to the development of OCD. However, more research is needed to better understand the connection between the two.
Triggers of OCD can be different for everyone. Things that cause stress or anxiety are often triggers of OCD.
Common triggers can include:
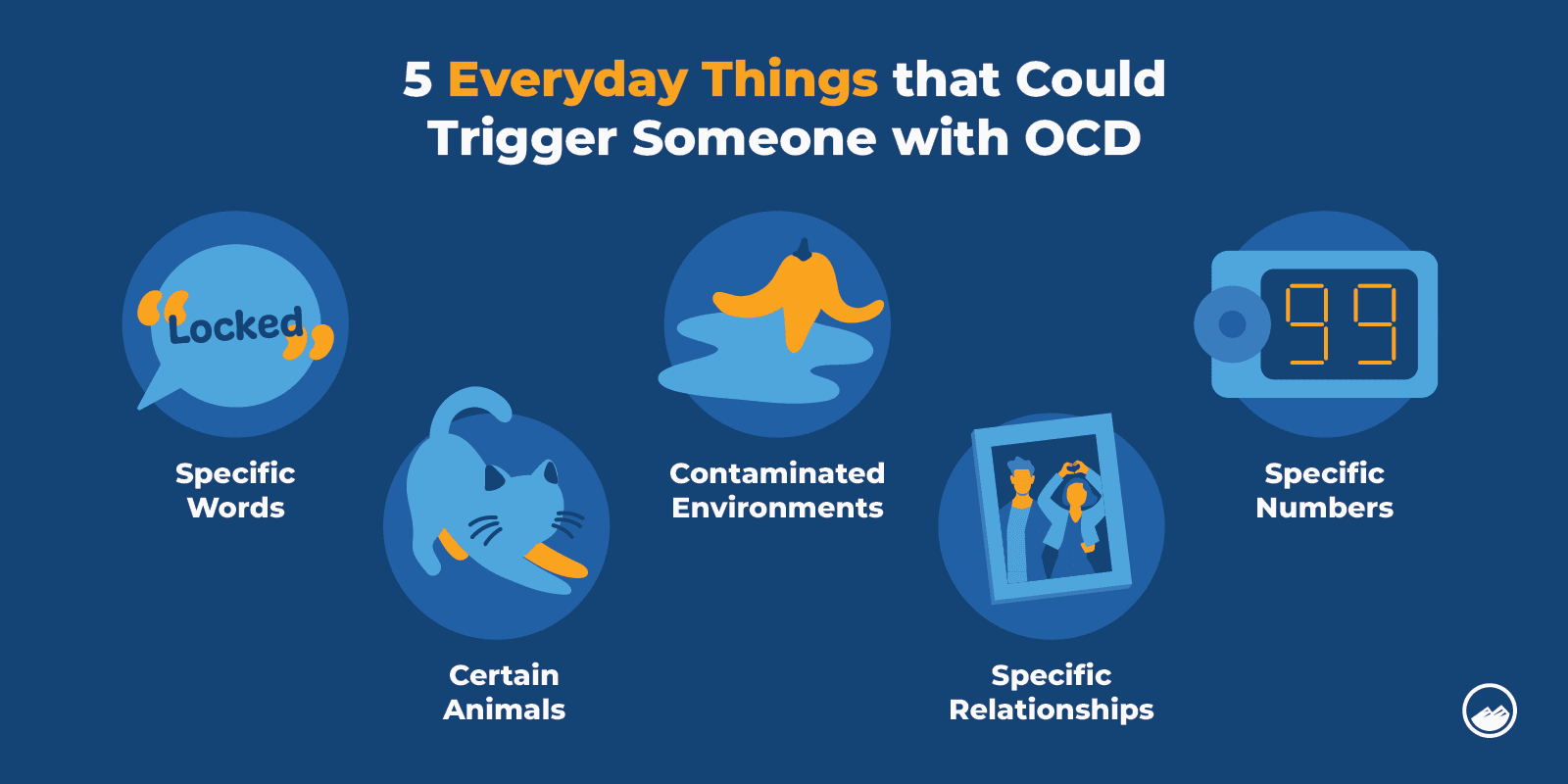
Various types of abuse may cause or trigger OCD, such as bullying, childhood trauma, emotional neglect, and sexual abuse.
Sometimes, OCD can stem from traumatic experiences, especially during childhood. As a result, a person might learn to use obsessions and compulsions to cope with these traumatic experiences.
Some individuals may also use obsessions and compulsions to cope with anxieties, especially if they’ve seen a parent or family member cope using similar techniques.
Individuals with OCD can have symptoms of obsessions, compulsions, or a combination of both.
Obsessions and compulsion are defined as:
There are often elaborate rules in regards to how they must be performed. The compulsion(s) take up a significant amount of time and keep the person from participating in his or her life. While the person may be aware of the behaviors, they might not seem them as abnormal and there is usually no attempt to hide them.
Common signs and symptoms of OCD obsessions can include:
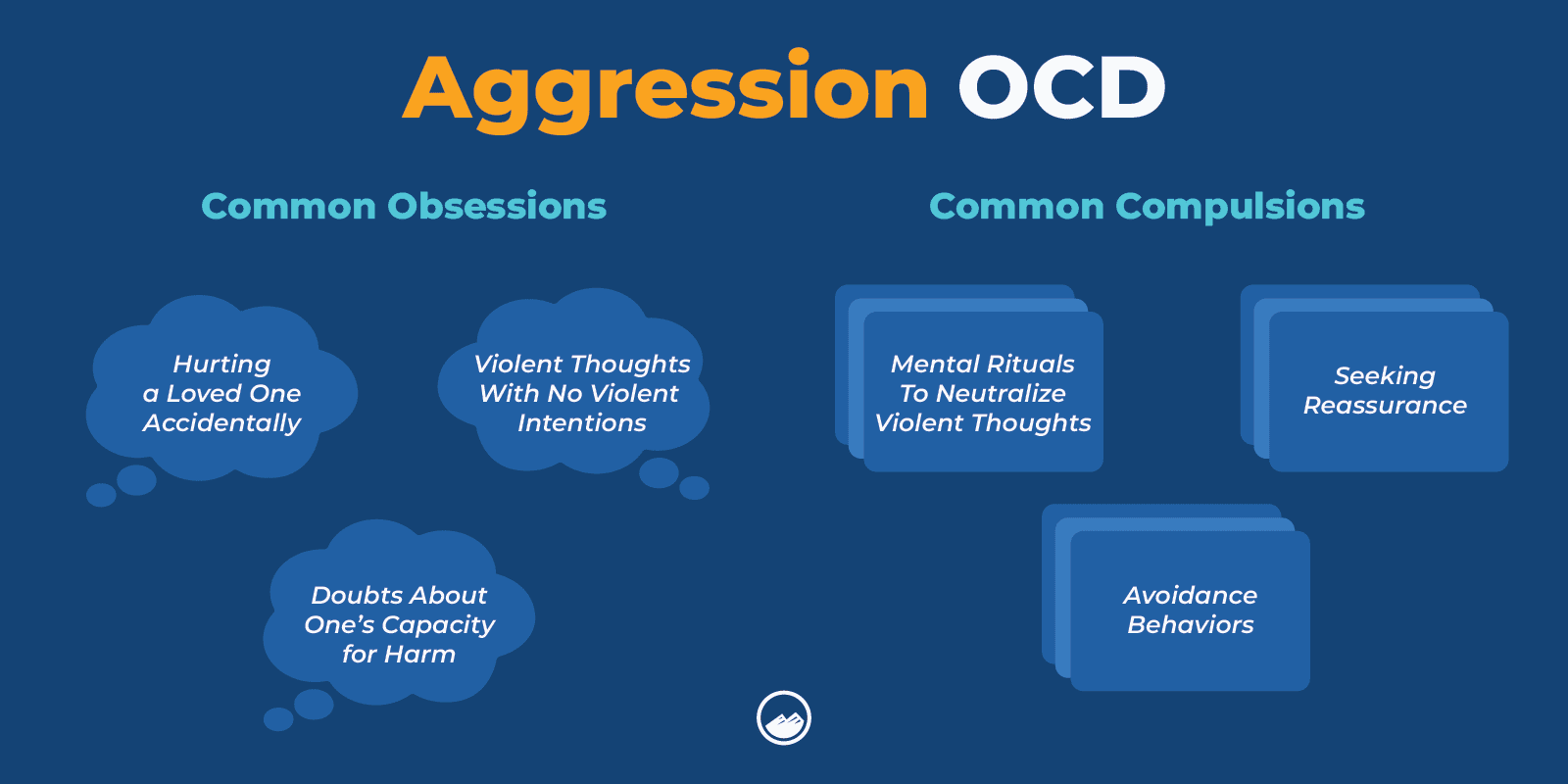
Common signs and symptoms of OCD compulsions can include:
Individuals with OCD can have entirely different habits from one another, but common ones may include:
OCD habits can become very time-consuming and impact a person’s daily routine and life.
When a person experiences, an OCD thought, it is often described as their brain and thoughts feeling out of control. OCD thoughts can be very distressing and disturbing.
For example, a person experiencing OCD thoughts may think of:
Some common symptoms of compulsions and obsessions in OCD can include:
The biggest symptoms of OCD are obsessions and compulsions that impact everyday life.
OCD can affect people in many different ways.
Obsessions and compulsions can cause distressing feelings that lead to feelings of anxiety, depression, and overall stress that can be very difficult to manage.
Some people may become avoidant to isolate themselves from triggers or hide their symptoms because they feel ashamed or embarrassed.
Avoiding treatment can make symptoms worse and increase the isolation someone with OCD already experiences. If you or a loved one struggle with OCD or have resonated with the symptoms listed in this article, it is important to reach out to a mental health professional.
Some people may experience more moderate symptoms of OCD, while others may have more severe symptoms.
OCD is a chronic disorder that can interfere with a person’s daily life, relationships, and personal view of themselves and the world around them. Some people with OCD may find that they have a diminished quality of life, especially when symptoms are untreated or undiagnosed.
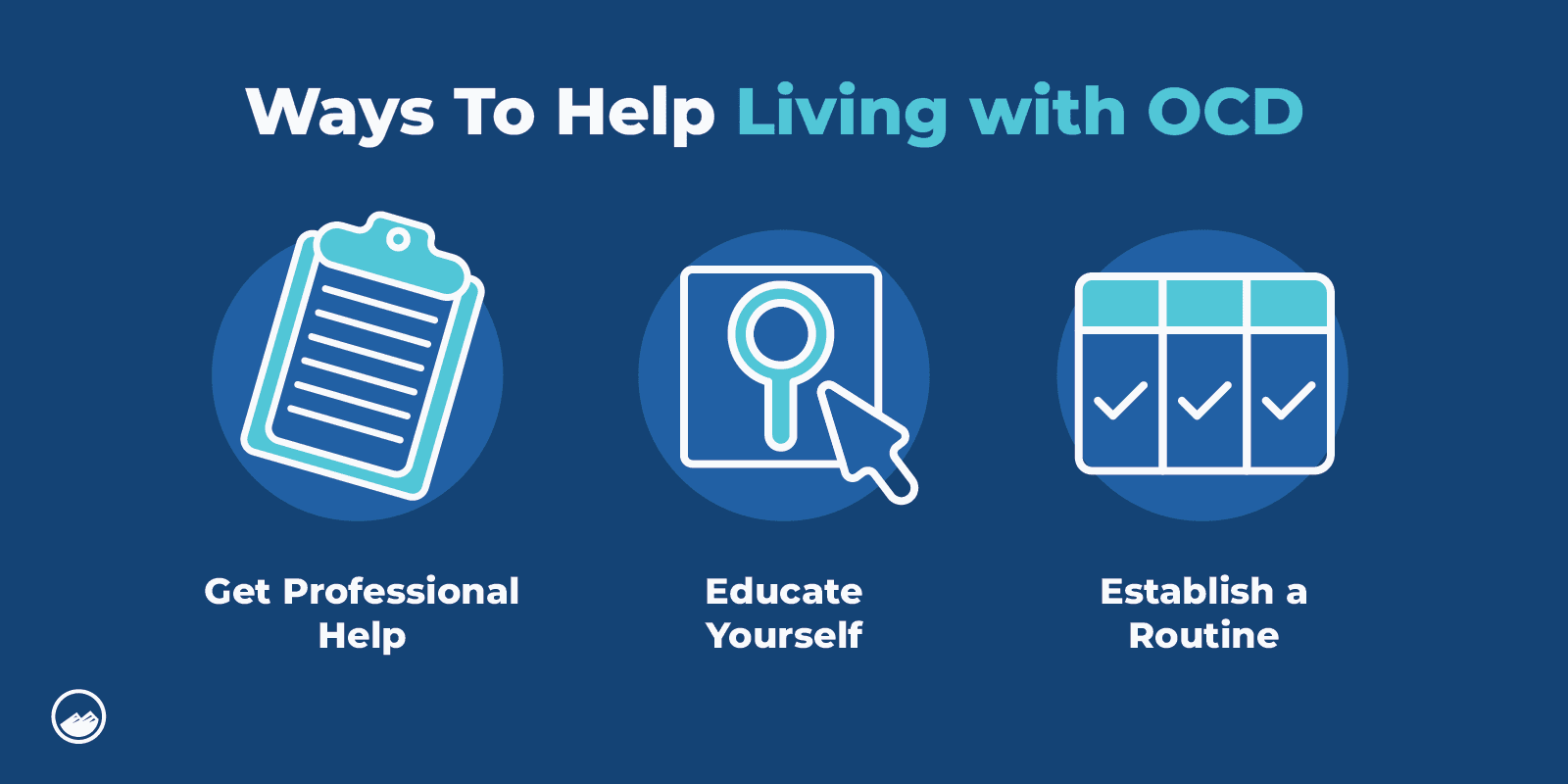
With the proper treatment, individuals with OCD can find ways that work for them in coping and managing their symptoms and living a healthy and fulfilling life.
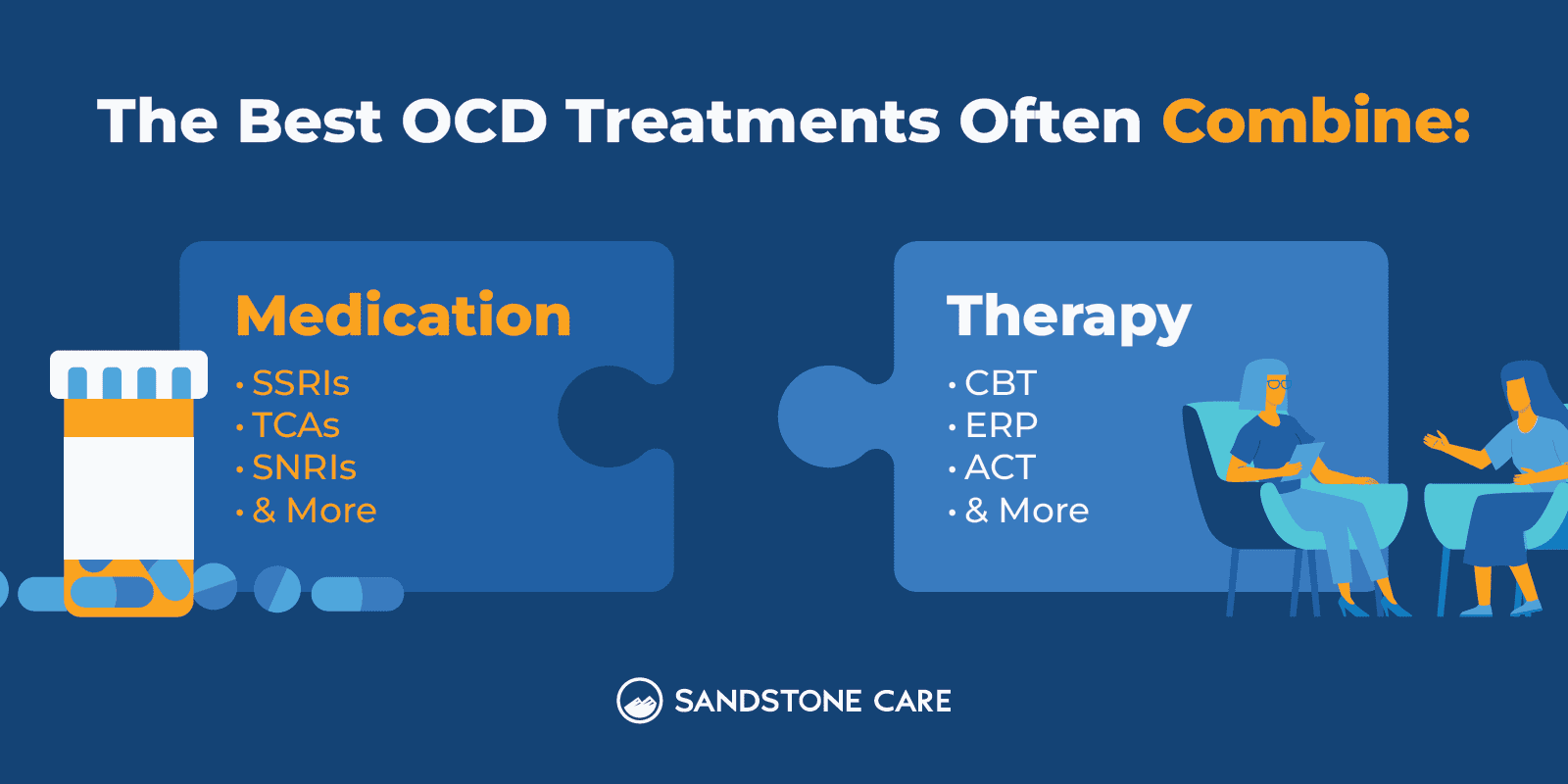
Treatment may include medications such as antidepressants, therapies such as exposure therapy, or other interventions such as deep brain stimulation.
According to Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, individuals with obsessive-compulsive disorder often experience emotions such as “anxiety, fear, and disgust” as a response to obsessive thoughts, urges, or images.
These emotions contribute to the action of engaging in compulsions as a way to remedy the difficult feelings that can come with obsessions. Individuals may anticipate something horrible or devastating to happen, so they engage in their compulsions to try to prevent the anticipated outcomes.
OCD can impact a person’s relationships and social life.
Some people with OCD choose to avoid intimate relationships to prevent the stress that comes with certain situations in daily life and relationships.
Sometimes, a person with OCD will need more reassurance in a relationship. A person with OCD may have a fear of something bad or losing their partner, which can make OCD symptoms challenging to manage.
It is important for partners of individuals with OCD to educate themselves so they can better understand how OCD works and how they can help their loved one in creating a safe, trusting, and healthy place.
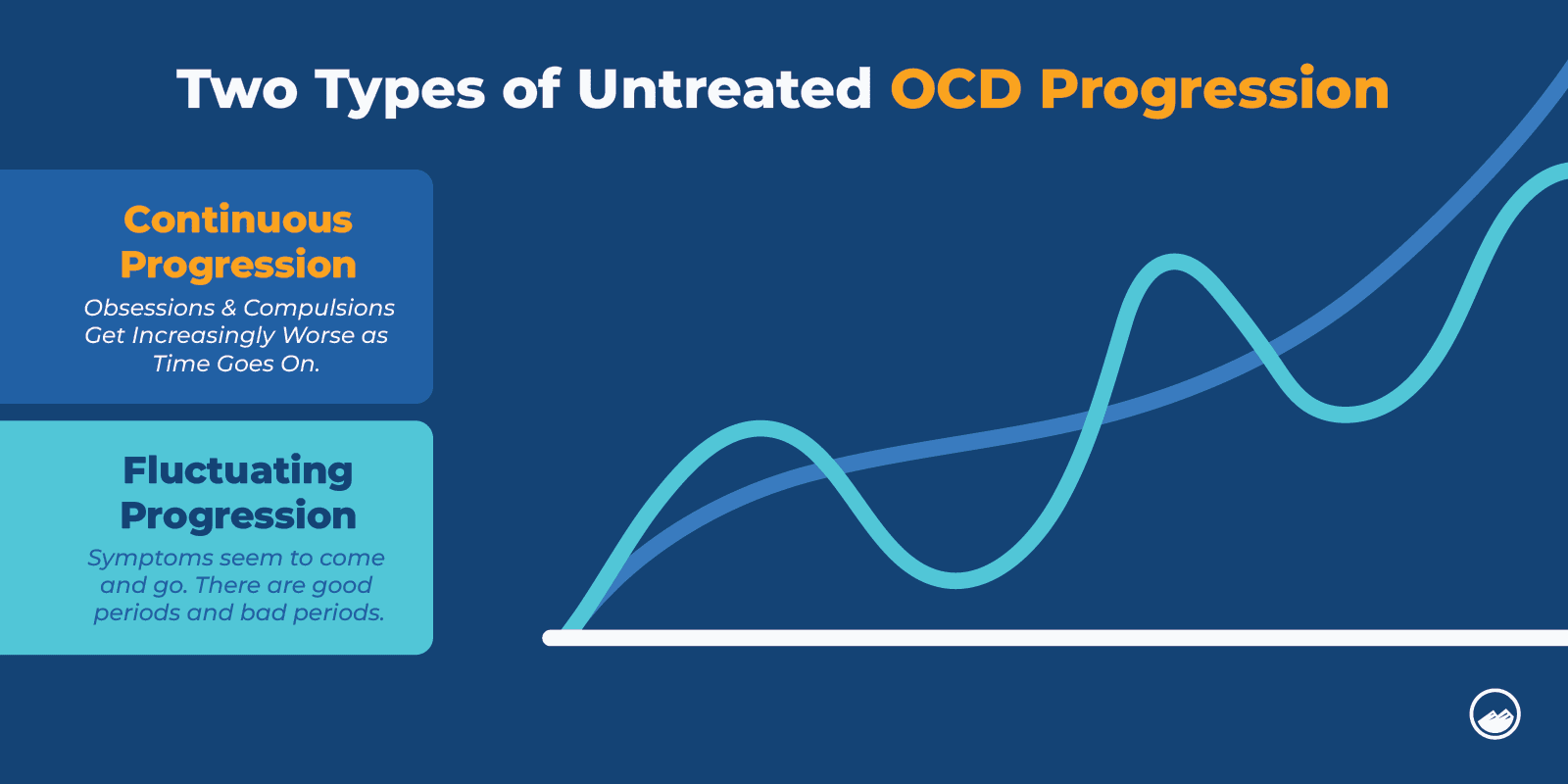
If left untreated, OCD can get worse with age.
OCD is described as a chronic, lifelong disease, however, a person may have periods varying in severity. Stressful life events, specific triggers that precipitate anxiety or general increases in stress may all bring on a period of increased symptomatology.
The average age of onset is 19 years old, however, a person can show symptoms and and develop the disorder as a young child. OCD does not present past the age of 35.
Symptoms of OCD can also fluctuate over different periods, and it is possible that some symptoms get worse with age.
Brain scans can show abnormalities in brain activity in individuals diagnosed with OCD.
Magnetic resonance imaging (MRI) has shown that individuals without OCD have smaller orbitofrontal cortex volumes than individuals with OCD.
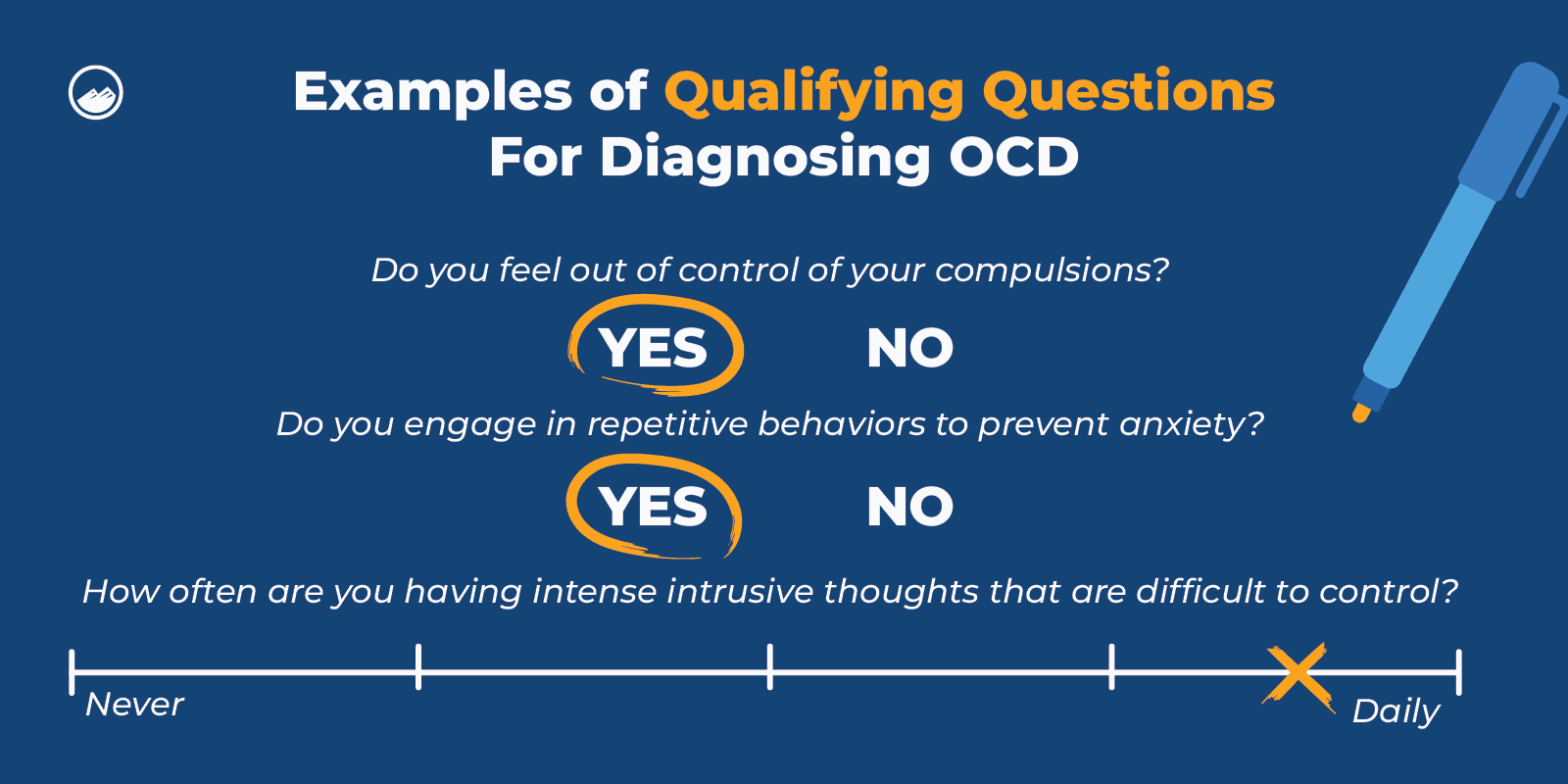
There is no specific test for OCD.
However, a healthcare provider can diagnose OCD based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria.
When diagnosing a person for OCD, a professional will go through a thorough assessment and evaluation to help rule out any other possibilities and ask about a person’s symptoms, medical history, and mental health history.
When OCD goes undiagnosed and untreated over time, it can become more severe and difficult to manage.
OCD symptoms may present themselves in various ways when undiagnosed.
For example, a person may experience very distressing thoughts and feelings that seem to come out of nowhere and that they don’t know how to get rid of. They may get caught in cycles of unhealthy behaviors or start to isolate themselves from others because they are unsure of how to cope with these challenges.
It is important to reach out for help if you think you or a loved one may have undiagnosed OCD.
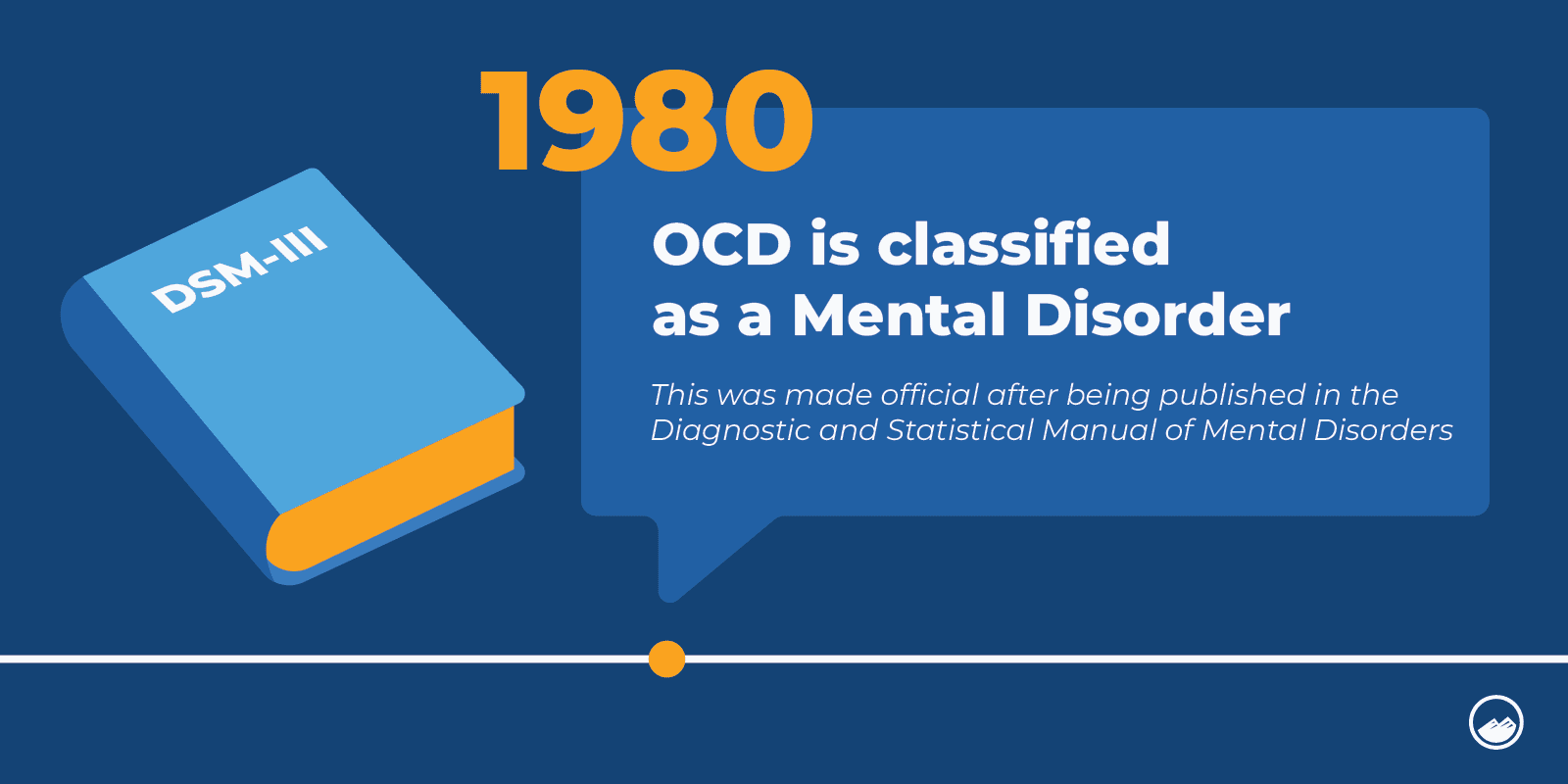
In the past, OCD was classified as a type of anxiety disorder. Now, OCD is designated by the American Psychiatric Association (APA) as its separate mental health condition.
Selective serotonin reuptake inhibitors (SSRIs) are commonly recommended to treat OCD as they are considered safe and effective.
Many SSRIs also have fewer side effects than alternative medications.
Selective serotonin reuptake inhibitors such as sertraline, fluoxetine, and paroxetine are some of the most common and effective OCD medications and are also FDA-approved.
When considering medications, it is important to discuss the risks and safety of your personal needs with your healthcare provider to come up with the best plan that works for you.
In some cases, if SSRIs don’t work, research shows that some individuals may do well with antipsychotic medications.
Medication can be an effective treatment for many individuals with OCD.
Treating OCD often combines medication with psychotherapy or talk therapies, like cognitive behavioral therapy (CBT).
The most common and effective SSRIs for OCD can include:
Treatment for OCD is different from person to person.
However, OCD treatment most commonly involves psychotherapy or talk therapy.
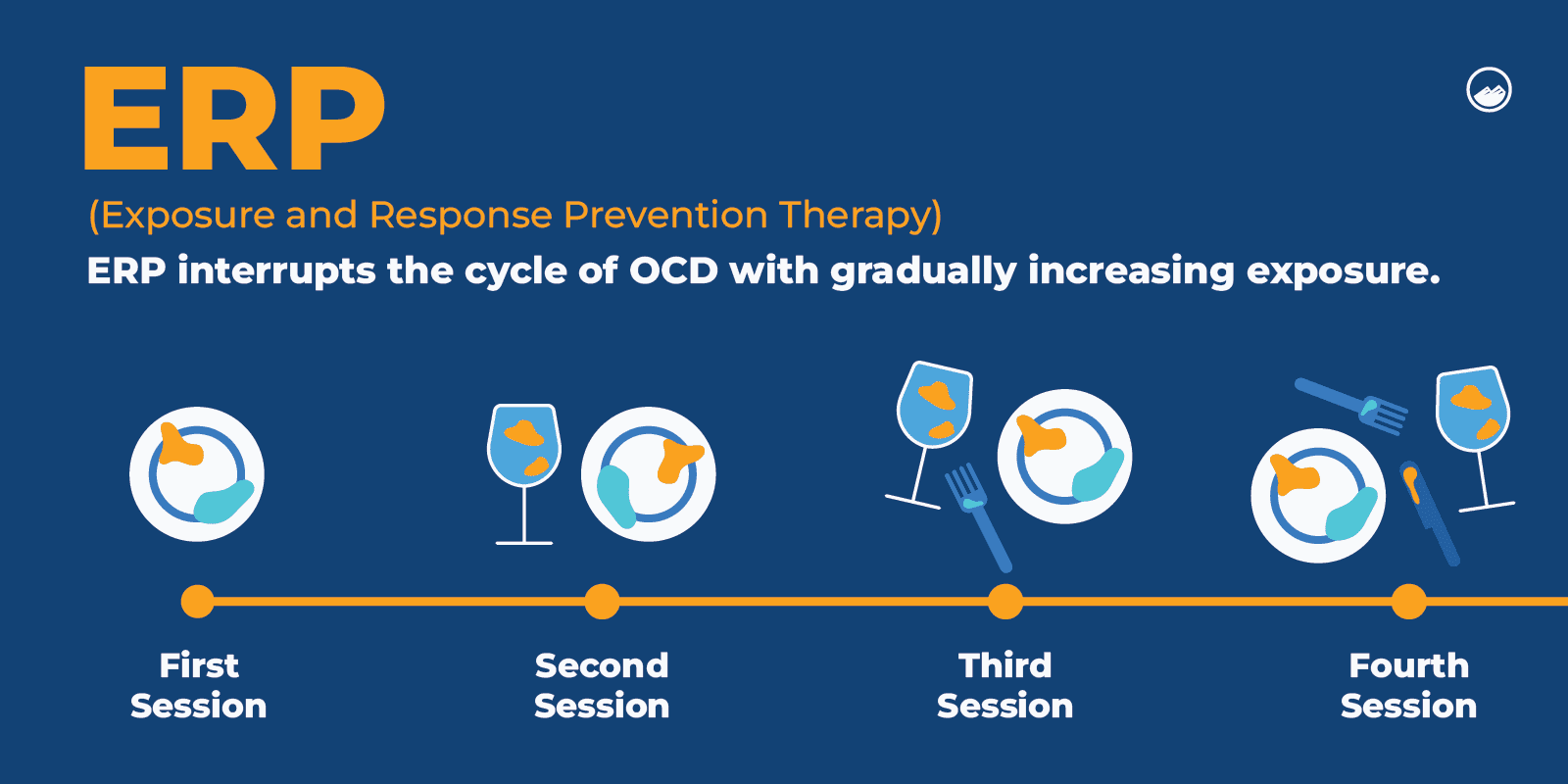
Exposure and response prevention (ERP) is a type of cognitive behavioral therapy that helps a person confront their fears and triggers and work on managing them so that they can gain control over their obsessions and compulsions.
Cognitive behavioral therapy (CBT), in general, can help a person learn to identify and address unhealthy thought and behavior methods, understand the meanings associated with them, and work on restructuring and changing them.
The best treatment for OCD is the one that works for the individual. This may mean medication, psychotherapy, both, or another treatment approach, like transcranial magnetic stimulation.
There is no cure for OCD, but getting professional help can help a person manage and cope with their symptoms and improve their quality of life.
Exposure and response prevention (ERP) is a type of cognitive behavioral therapy (CBT) that can help a person learn how to confront and manage their triggers.
Support groups can also provide a safe and welcoming place for individuals with OCD to relate to others and build strong connections with people who may share similar experiences with them.
Over time, if OCD is left untreated, symptoms can become worse and lead to severe mental health conditions, such as anxiety, depression, panic attacks, and suicidal thoughts.
There is no known cure for OCD.
However, many people can manage and cope with their symptoms, function well daily, and live happy, fulfilling lives.
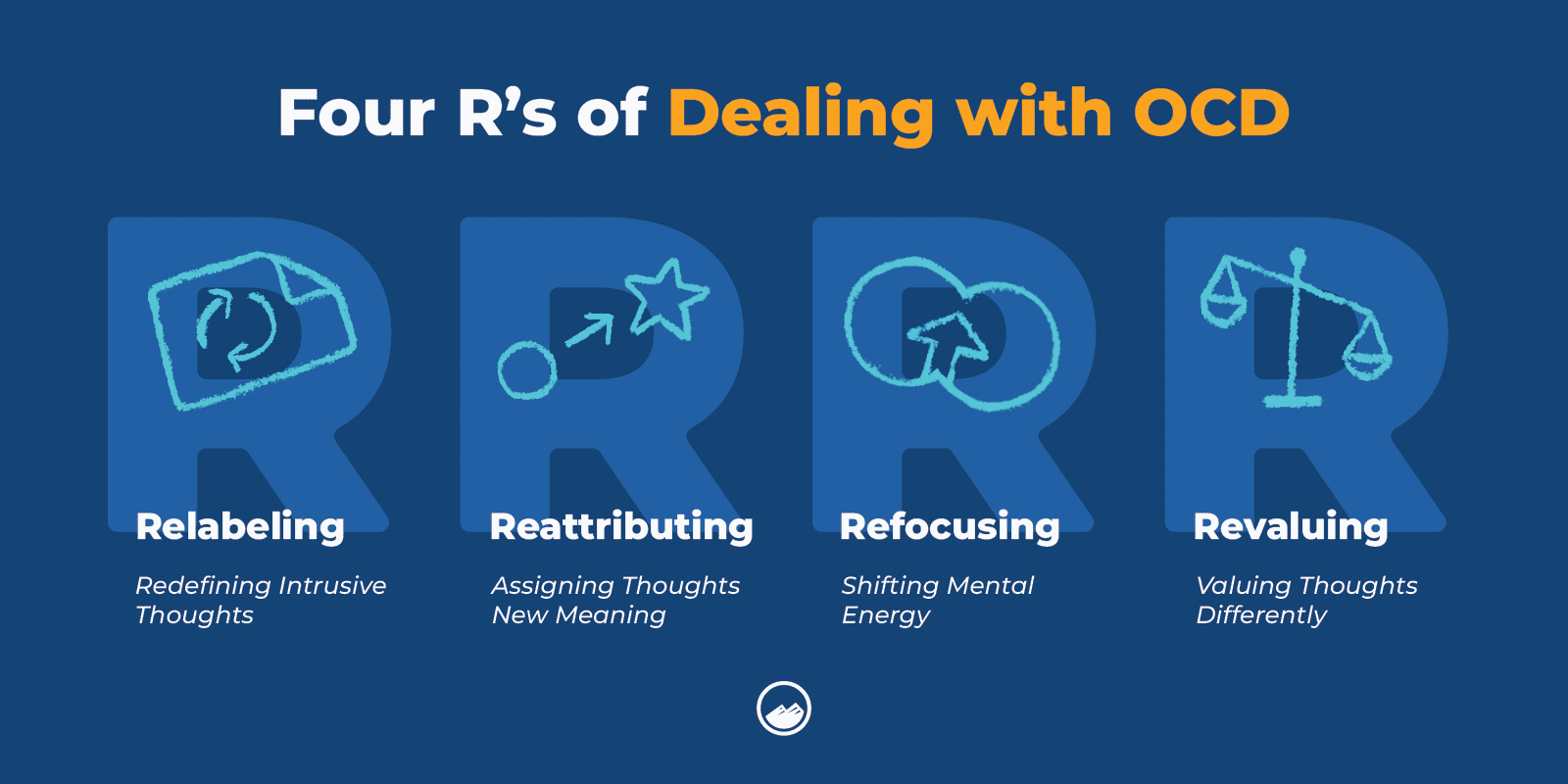
The four R’s are a technique developed to help aid in OCD treatment.
The four R’s stand for:
OCD thoughts can cause a person to feel very overwhelmed, stressed, and anxious.
Some tips and techniques a person can use to help calm OCD thoughts can include:
The three C’s of cognitive therapy that are used to help manage symptoms of OCD include:
FAQ
Our goal is to provide the most helpful information. Please reach out to us if you have any additional questions. We are here to help in any way we can.
Depression is a mood disorder that affects how a person thinks and feels and how they go through everyday life.
Depression is characterized by persistent feelings of sadness.
OCD and depression can share similar signs and symptoms, such as upsetting thoughts, negative feelings toward oneself, or negative thinking patterns. It is also not uncommon for individuals to be diagnosed with OCD and depression.
Various types of experiences from childhood may contribute to the development of OCD.
Forms of childhood trauma that may cause OCD can include child maltreatment, emotional neglect, or abuse.
OCD is likely linked to low levels of serotonin. However, more research is needed to understand the connection between the two.
According to MedlinePlus, “the inheritance pattern of OCD is unclear.” However, the risk of developing OCD is higher in individuals with first-degree relatives, like siblings or parents, who have been diagnosed with OCD.
OCD and autism may share a few similar symptoms. However, OCD is a mental health disorder, and autism is a developmental condition.
It is believed that famous geniuses like Charles Darwin and Nikola Tesla have been diagnosed with OCD.
It can be very challenging to live with OCD, and this diagnosis is often misunderstood.
OCD can be debilitating, which is one of the reasons why it is so important that a person gets the best support available.
Those with OCD can be at specific risk for using substances, particularly with alcohol and marijuana abuse, to help alleviate or escape their disorder.
With fear and anxiety playing such a strong role in the structure of the disorder, it is unsurprising that those with OCD can seek out other methods to try to reduce their overall anxiety or decrease their OCD behaviors.
The risks around alcohol & marijuana abuse for those with OCD significantly increase when they are linked to another co-occurring disorder.

Obsessive-compulsive disorder (OCD) is a chronic disorder that involves obsessions and/or compulsions that can interfere with a person’s daily life. Sandstone Care is here to support teens, young adults, and adults with mental health and substance use disorders. Call (888) 850-1890.