Different Types of OCD
What Type of Disorder Is OCD?
Obsessive-Compulsive Disorder (OCD) is classified as an anxiety disorder.
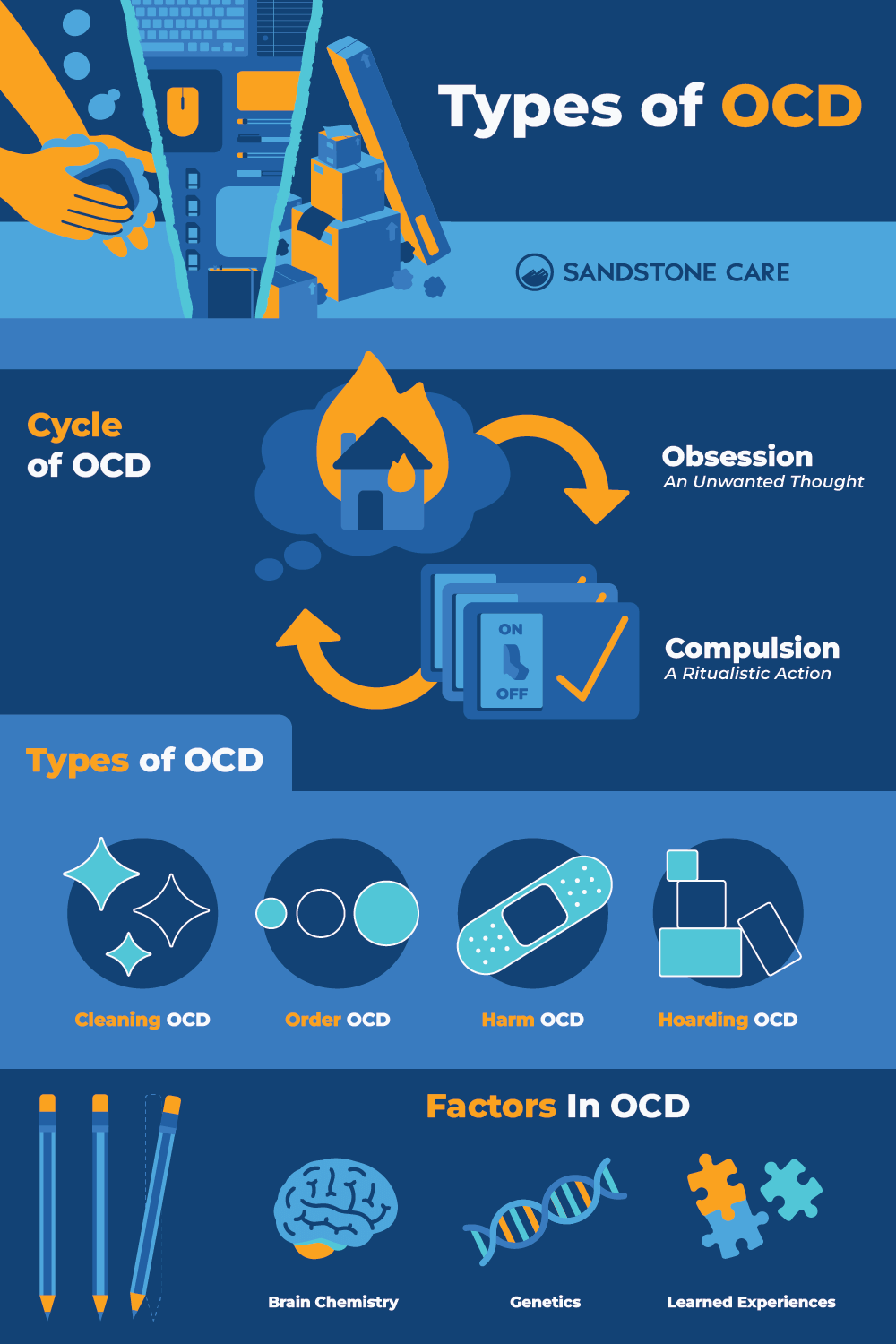
People with Obsessive-Compulsive Disorder (OCD) experience distressing, unwanted thoughts that drive them to perform repetitive and ritualistic actions to reduce the anxiety triggered by these thoughts.
Are There Different Types of OCD?
OCD is a very complex disorder that can manifest itself in various ways. There are different types of OCD, but some people may not fall into just one category.
It’s important to note that while the specific obsessions and compulsions may vary, the underlying mechanism of anxiety and obsession-driven behaviors is in all types.
How Many Types of OCD Are There?
OCD generally falls into four different categories, but some people categorize it into 7 or even 13 different categories.
Categories range from common OCD themes such as contamination OCD, which often leads to cleaning compulsively, to more specific themes such as scrupulosity, which centers around moral and religious obsessions.
Some types manifest differently than others. For example, “Pure O” OCD is centered almost entirely on mental obsessions, and less on behaviors.
What Are the Different Types of OCD?
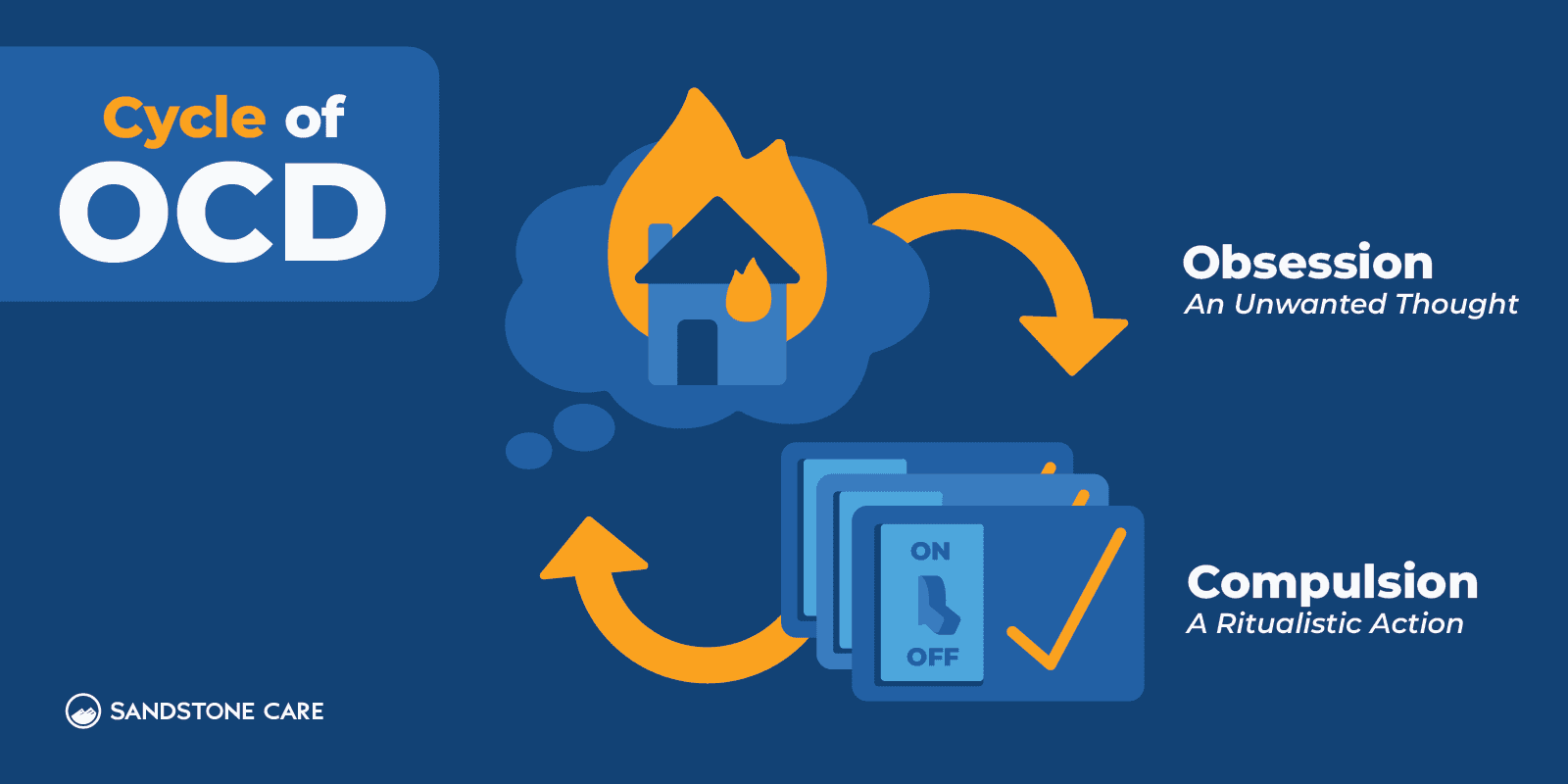
The four most common types of obsessive-compulsive disorder include cleaning/contamination OCD, order/symmetry OCD, harm OCD, and hoarding OCD.
Here is a more thorough breakdown of these four types and how they appear in daily life:
- Cleaning/Contamination OCD
This type involves obsessive fears of germs, dirt, or contamination, which lead individuals to engage in compulsive cleaning or avoidance behaviors. - Order/Symmetry OCD
People with this subtype have obsessions related to achieving perfection, symmetry, or exactness. Compulsions often involve arranging and organizing items to meet these standards. - Harm OCD
Individuals with harm OCD experience distressing thoughts or fears about causing harm to themselves or others. Compulsions may include checking behaviors to make sure nothing bad has happened. - Hoarding OCD
Hoarding involves difficulty discarding possessions, even when they have no practical value. This can lead to excessive clutter and a reluctance to part with items.
What Is the Most Common Type of OCD?
Contamination OCD is the most commonly seen subtype of OCD.
Can You Have Multiple Types of OCD?
Yes, OCD is a complex disorder, and individuals with OCD may experience symptoms that don’t fall under simply one type of OCD.
Many people with OCD experience symptoms of multiple types of OCD. They also often experience related disorders and mental illnesses that can make it difficult to pin down a diagnosis at first.
What Part of the Brain Is Triggered by OCD?
Studies suggest that the prefrontal cortex, basal ganglia, and thalamus are all triggered by OCD.
Contamination OCD with Washing/Cleaning Compulsions
What Is Contamination OCD?
Contamination OCD is a type of OCD that involves the fear of contamination, contaminating others, or spreading germs.
People who have Contamination OCD often have very upsetting thoughts about germs or dirt, even in situations that most people wouldn’t worry about. These thoughts make them feel extremely anxious and uncomfortable.
Obsessions and compulsions may include:
Obsessions: Fear of germs, dirt, or other contaminants.
Compulsions: Excessive hand-washing, showering, or cleaning objects.
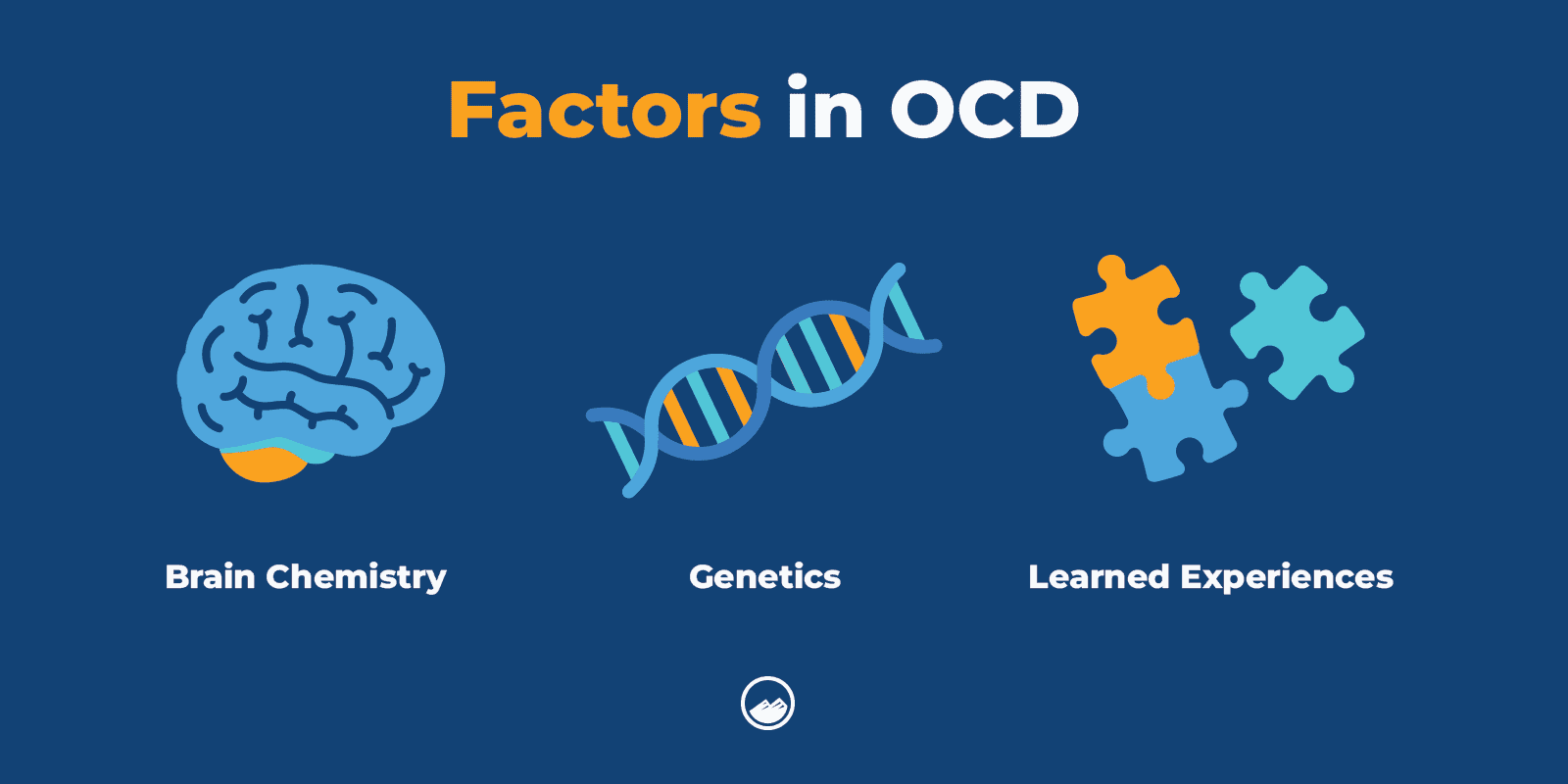
What Causes Contamination OCD?
The causes of OCD, including contamination OCD, are unknown. However, factors like brain chemistry, genetics, and learned experiences may play a role.
How to Beat Contamination OCD?
One of the most common treatment approaches for contamination OCD is exposure and response prevention (ERP) therapy.
In ERP therapy, an individual with contamination OCD gradually faces their fears. Then, they will actively try not to engage in their compulsion.
For example, a person who is nervous about the contamination of a doorknob may gradually try to touch it without washing their hands immediately after. As they get better, they will be able to delay the time between touching the doorknob and washing their hands to help loosen the power of their compulsion.
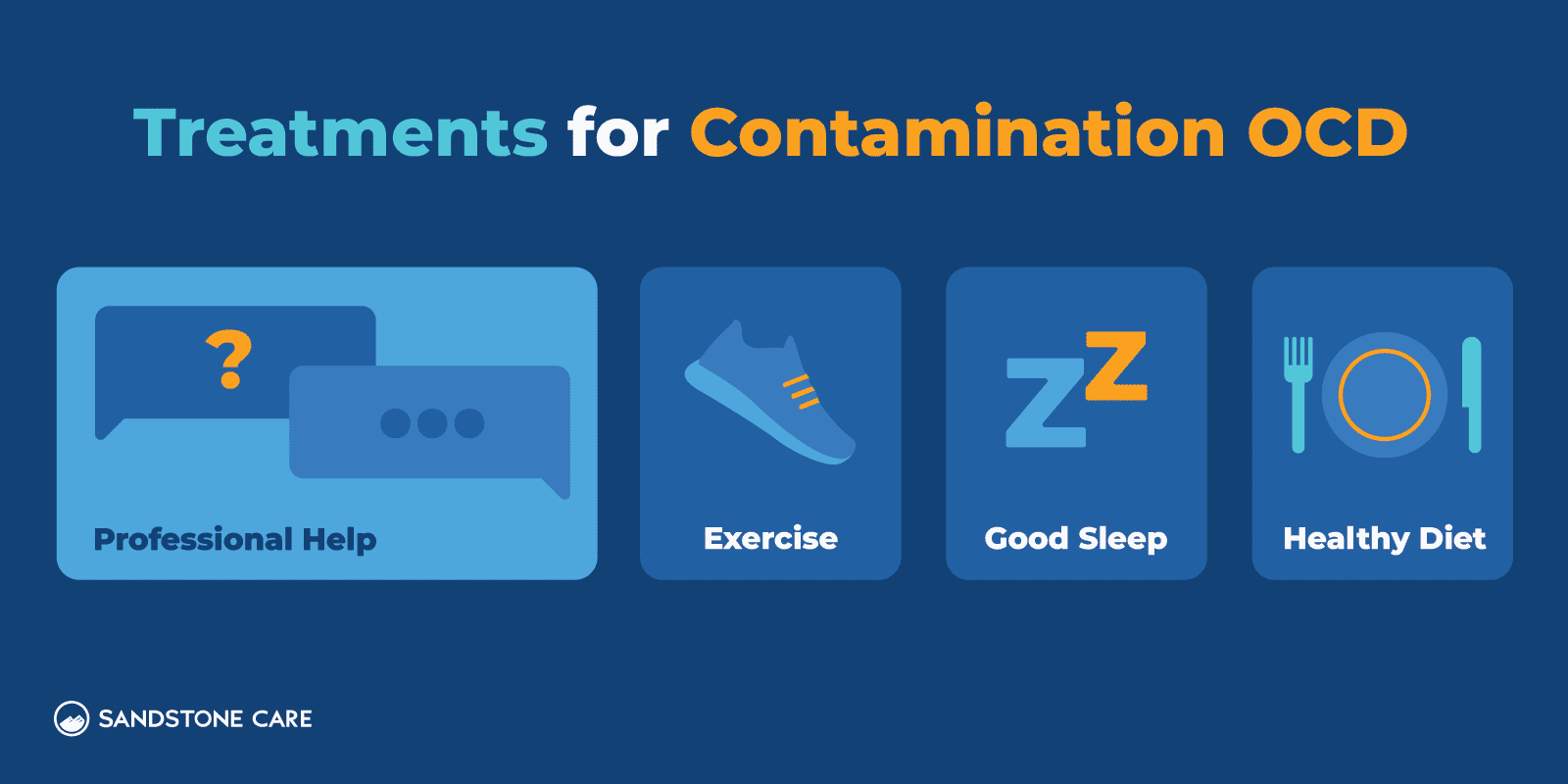
How to Treat Contamination OCD at Home?
If a person is diagnosed with contamination OCD, it is best to receive professional help and not try to treat yourself.
However, there are things a person can do outside of therapy that may help them manage symptoms and triggers of contamination OCD.
Managing stress and practicing healthy habits such as getting physical exercise, eating a balanced diet, and getting good rest can help a person minimize triggers and ruminations that worsen the symptoms of OCD.
How to Help Someone With Contamination OCD?
If a loved one may have contamination OCD, it is best to connect with professional help to get a proper diagnosis and guidance on how you can help them.
Going through therapy for contamination OCD can be challenging in everyday life, and having someone there who encourages and supports them can make all the difference. You can also attend support groups with them so that they can build a network of people who understand what they’re going through.
Checking OCD
What Is Checking OCD?
Checking OCD is a form of OCD that involves checking and rechecking things to feel less afraid that something bad will happen.
These rituals are used to reduce feelings of uncertainty that can feel unbearable.
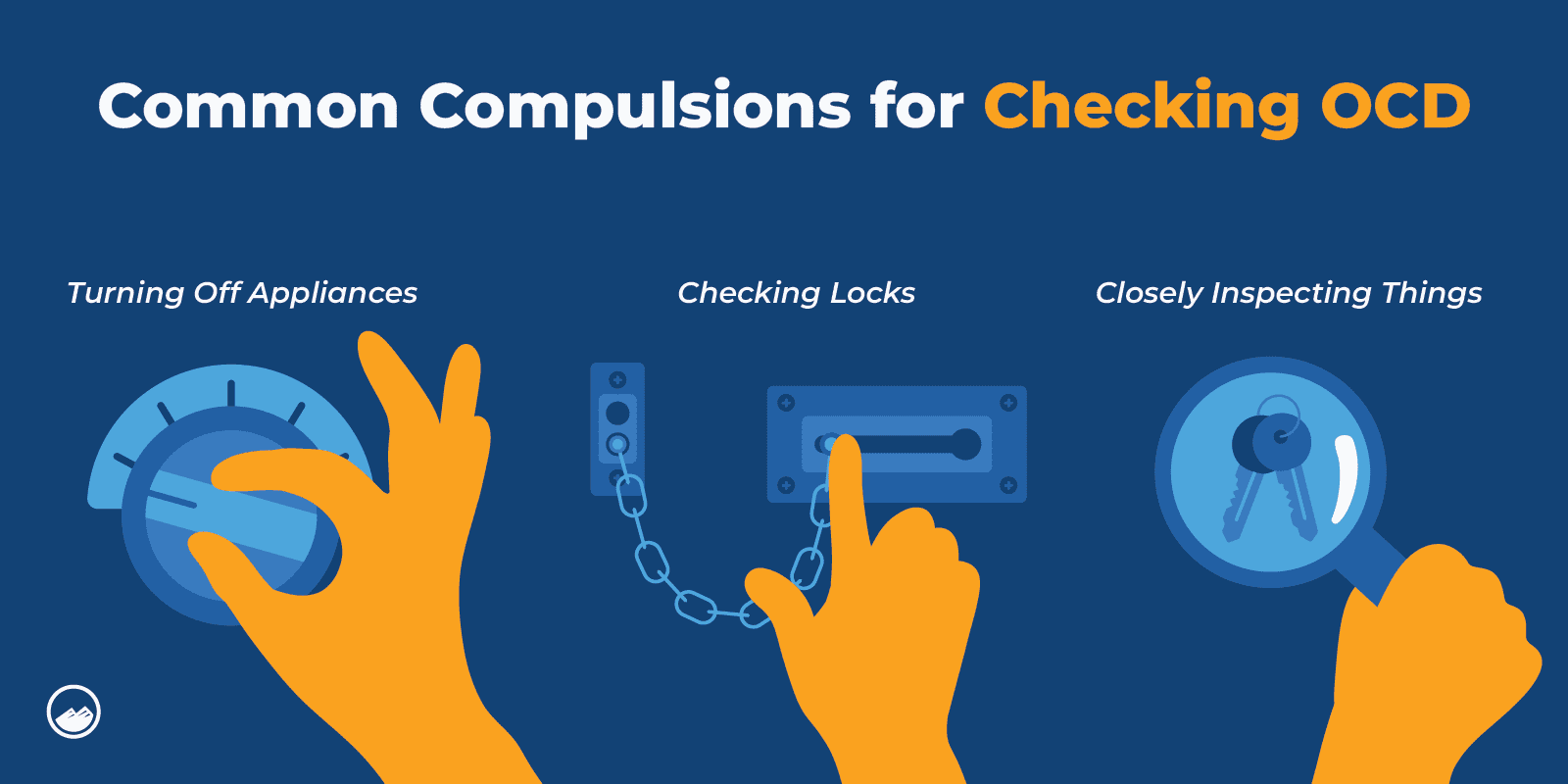
Some obsessions and compulsions with this type may include:
Obsessions: Fear of something bad happening, experiencing intrusive thoughts that they are not doing something that prevents harm, fear that they lost something.
Compulsions: Repetitively checking if they turned off appliances, repeatedly making sure things are locked, closely inspecting things.
What Triggers Checking OCD?
Everyone’s triggers can be different. However checking OCD is often triggered by a fear that something bad will happen to themselves or another person if they don’t check and recheck what they are worried about.
Some triggers may include fearing that they accidentally left the oven on or forgot to change the batteries in the smoke detector.
What Does OCD Checking Feel Like?
A person with OCD checking may often feel anxious, worried, or stressed that something terrible is going to happen if they don’t engage in their compulsions.
These ruminations can feel inescapable, which can make the sufferer isolate themselves from other people. They also may experience intrusive thoughts and different symptoms of anxiety.

Why Is OCD Checking Bad?
OCD checking is unhelpful because it impacts a person’s ability to function in daily life, which can destroy their confidence.
OCD checking also leads to more compulsive behaviors that can take up a lot of a person’s life energy. This can also make it difficult for them to have healthy social lives and careers if their checking compulsions are severe.
How Do You Stop OCD Checking?
Cognitive behavioral therapy (CBT), like exposure and response prevention therapy, can help a person learn to challenge their thoughts and not give in to their compulsions.
Speaking to a professional in the psychiatry and psychology field can help them to find the specific resources they need to break the cycle of obsessive and compulsive checking.
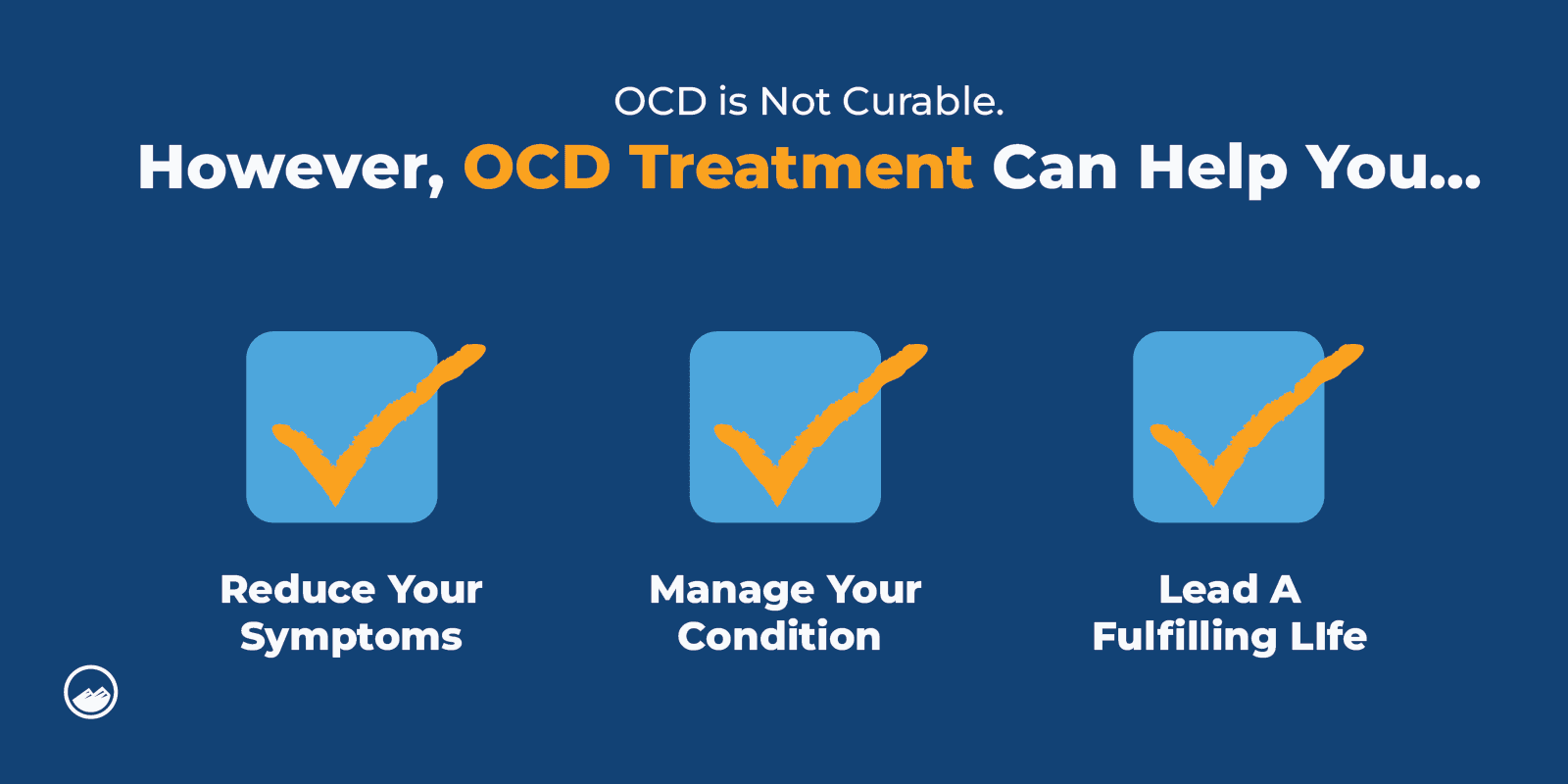
Is Checking OCD Curable?
OCD is not curable, but it is treatable.
Obsessive-Compulsive Disorder (OCD) is considered a chronic condition, which means that it typically does not have a complete “cure.” However, with appropriate treatment, many individuals with OCD can significantly reduce their symptoms, manage the condition effectively, and lead fulfilling lives.
Does OCD Go Away if You Ignore It?
OCD does not just go away on its own. Often by trying to ignore OCD, obsessions can become stronger, which can cause a cycle of distress and worsening symptoms.
OCD is a mental health condition that almost always requires professional treatment.
Harm OCD With Checking Compulsions
What Is Harm OCD?
Harm OCD involves intrusive and obsessive thoughts or images of harming oneself or others.
These intrusive moments can involve violent or sexual thoughts, even when the sufferer has no intent of ever acting on those images.
Some of the obsessions and compulsions that may happen with this type include:
Obsessions: Thoughts or images related to hurting or inflicting violence onto oneself or another person.
Compulsions: Seeking reassurance, mental rituals, and/or avoidance.
What Causes Harm OCD?
Harm OCD, like other types of Obsessive-Compulsive Disorder (OCD), doesn’t have a single, simple cause.
Instead, researchers have found that it likely develops from a mix of different biological, social, and personal circumstances.
Factors that may contribute to the development of harm OCD can include:
- Traumatic or stressful life events
- Family history of OCD
- Differences in brain structure or functioning
- Co-occurring mental health disorders
What Are Harm OCD Symptoms?
Common harm OCD symptoms can include:
- Worrying that they will harm themselves or someone else
- Fear of becoming violent
- Fear of following through on an intrusive obsession
- Fear of committing suicide
If you or a loved one are experiencing suicidal thoughts, call the National Suicide Prevention Lifeline at 988 or call 911.
Is Harm OCD Dangerous?
Often, a person with harm OCD doesn’t carry out their thoughts of physical harm.
However, OCD can increase a person’s risk of becoming suicidal or self-harming as a coping mechanism to stop their intrusive thoughts.
How Common Is Harm OCD?
According to studies, harm OCD is one of the most common forms of OCD.
Sometimes people with harm OCD are embarrassed or afraid to tell others about their experiences, so it is also likely underreported.
How to Overcome Harm OCD?
The first step to overcoming harm OCD is to reach out to a professional.
Getting professional help can give a person the tools and guidance they need to regain control of their life and learn to manage the symptoms of harm OCD.
Symmetry and Orderliness OCD With Ordering/Arranging Compulsions
What Is Symmetry and Orderliness OCD?
With symmetry and orderliness OCD, a person fixates on how certain objects are positioned or arranged.
The compulsive behaviors associated with this subtype typically revolve around arranging, counting, or organizing objects repeatedly until they meet the specific criteria.
Obsessions and compulsions that may occur with this type include:
Obsessions: Need for things to be symmetrical, aligned, or in a specific order.
Compulsions: Repetitive behaviors arranging or ordering items until they feel “just right.”
What Triggers Symmetry OCD?
While everyone has different triggers, common triggers of symmetry OCD can include:
- Seeing objects arranged unevenly
- Seeing uneven facial features
- Experiencing a sensation on only one side of the body
- Walking in a way that doesn’t feel even
What Is an Example of Orderliness OCD?
An example of orderliness OCD may be seen in a person who becomes uncomfortable or even distressed if something doesn’t feel right. If their desk isn’t arranged the right way, if their car is not parked perfectly in the middle, or if objects aren’t arranged symmetrically even.
How Do You Treat Symmetry OCD?
The most effective treatment for Symmetry OCD, like other forms of OCD, is cognitive-behavioral therapy (CBT) with a specific focus on Exposure and Response Prevention (ERP).
Forbidden or Taboo Thoughts With Mental Rituals
What Are Taboo Thoughts and Mental Rituals?
Individuals with taboo thoughts and mental rituals experience unwanted thoughts related to religion, violence, or sexuality.
- Obsessions: Disturbing thoughts related to themes like harm, religion, or sexuality.
- Compulsions: Mental rituals or other cognitive strategies to counteract or neutralize the intrusive thoughts.
What Are Examples of Mental Rituals?
A mental ritual is when a person repeats certain mental actions to cope with the anxiety and feelings associated with their obsession.
An example of a mental ritual could be a person repeating special words, images, or numbers to reduce the anxiety that comes with their obsession.
How Do You Treat Taboo Thoughts and Mental Rituals?
Therapy, like CBT or ERP, can help a person manage their taboo thoughts and disengage with their mental rituals.
Hoarding OCD
What Is Hoarding OCD?
Hoarding OCD, sometimes referred to as hoarding disorder, is when a person has difficulty parting with or discarding things that don’t have an apparent value to them.
- Obsessions: Fear of throwing things away or losing something important.
- Compulsions: Accumulating items, often leading to clutter and dysfunction.
What Are the Symptoms of OCD Hoarders?
Common symptoms of OCD hoarders can include:
- Buying and keeping too many items that a person is running out of space for
- Difficulty getting rid of things, even if there is no value to them
- Feeling like they have to save items
Why Does OCD Cause Hoarding?
Some experts suggest that hoarding is caused by OCD because keeping things serves as a way for some individuals with OCD to manage certain obsessions and intrusive thoughts.
How Do You Overcome OCD Hoarding?
Reaching out to a therapist or another mental health professional can help a person overcome OCD hoarding.
Relationship OCD (ROCD)
What Is Relationship OCD?
Relationship OCD involves doubts and fears about a person’s relationship, most commonly in intimate and romantic relationships.
- Obsessions: Doubts about the suitability of a relationship partner or the relationship itself.
- Compulsions: Seeking reassurance, repeatedly checking feelings, or avoiding intimacy.
What Are the Symptoms of ROCD?
Common symptoms of ROCD include:
- Intrusive thoughts and whether or not their partner is right for them
- Going back and forth on whether or not they should end their relationship
- Doubting if their partner is attracted to them or if they are really attracted to their partner
What Is the Root Cause of ROCD?
The root cause of ROCD is unknown, but factors that may contribute can include genetics, environment, or traumatic life experiences.
What Triggers Relationship OCD?
Common triggers of relationship OCD can include boredom or distress with their partner when they see other couples or noticing a perceived flaw in their partner.
Somatic OCD
What Is Somatic OCD?
Somatic OCD, also known as sensorimotor OCD, is when a person has intrusive thoughts about autonomic bodily functions.
Obsessions: Excessive focus on bodily sensations or functions, such as breathing or blinking.
Compulsions: Checking the body, seeking reassurance, or avoiding certain situations.
What Are the Symptoms of Somatic OCD?
Common symptoms of somatic OCD can include:
- Focusing on one’s chewing
- Focusing on the way a person breathes
- Fixating and monitoring one’s heartbeat
- Focusing on blinking
What Triggers Somatic OCD?
Symptoms of somatic OCD are often triggered by intrusive thoughts that heighten someone’s awareness of bodily function.
What Does Somatic OCD Do?
Somatic OCD can cause a person to become hyper-aware and hyper-focused on autonomic processes such as breathing, blinking, or swallowing.
Is Somatic OCD Permanent?
Somatic OCD can be treated like other forms of OCD using approaches such as CBT or ERP.
Pedophilic OCD (POCD)
What Does POCD Mean?
A person with pedophilic OCD (POCD) experiences pedophilic obsessions.
- Obsessions: Intrusive, unwanted thoughts about harming children without intent or history of such behavior.
- Compulsions: Avoiding children, seeking reassurance, or performing mental rituals.
What Is a POCD Urge?
A POCD urge is when an individual experiences an obsessive impulse about harming children.
How Long Does POCD Last?
When left untreated, POCD can last a lifetime, which is why it is so important to reach out for help.
What Triggers POCD?
The most common trigger of POCD is being in a setting where children are present.
How Serious Is POCD?
POCD can cause serious, harmful impacts on a person’s life.
If you think you or a loved one might have POCD, it is crucial to reach out for professional help.
Why Do People Develop POCD?
The exact cause of POCD is unknown, but it is likely due to numerous factors, including genetics, environment, and brain structure and functioning.
How Do You Treat Pedophilic OCD?
POCD is most commonly treated using ERP.
Health or Illness OCD (Hypochondriasis)
What Is Hypochondria OCD?
Also sometimes referred to as health concern OCD, hypochondria OCD involves obsessions about having a serious, life-threatening medical condition.
- Obsessions: Fear of having a serious medical condition.
- Compulsions: Frequently checking the body for symptoms, seeking medical reassurance, or excessive research.
How Do You Know if You Have Health OCD?
Common compulsions of health OCD that can be signs can include:
- Frequently visiting the doctor or “doctor hopping”
- A habit of looking up symptoms online
- Frequently seeking more advanced testing
- Avoiding people or places where they may contract a disease
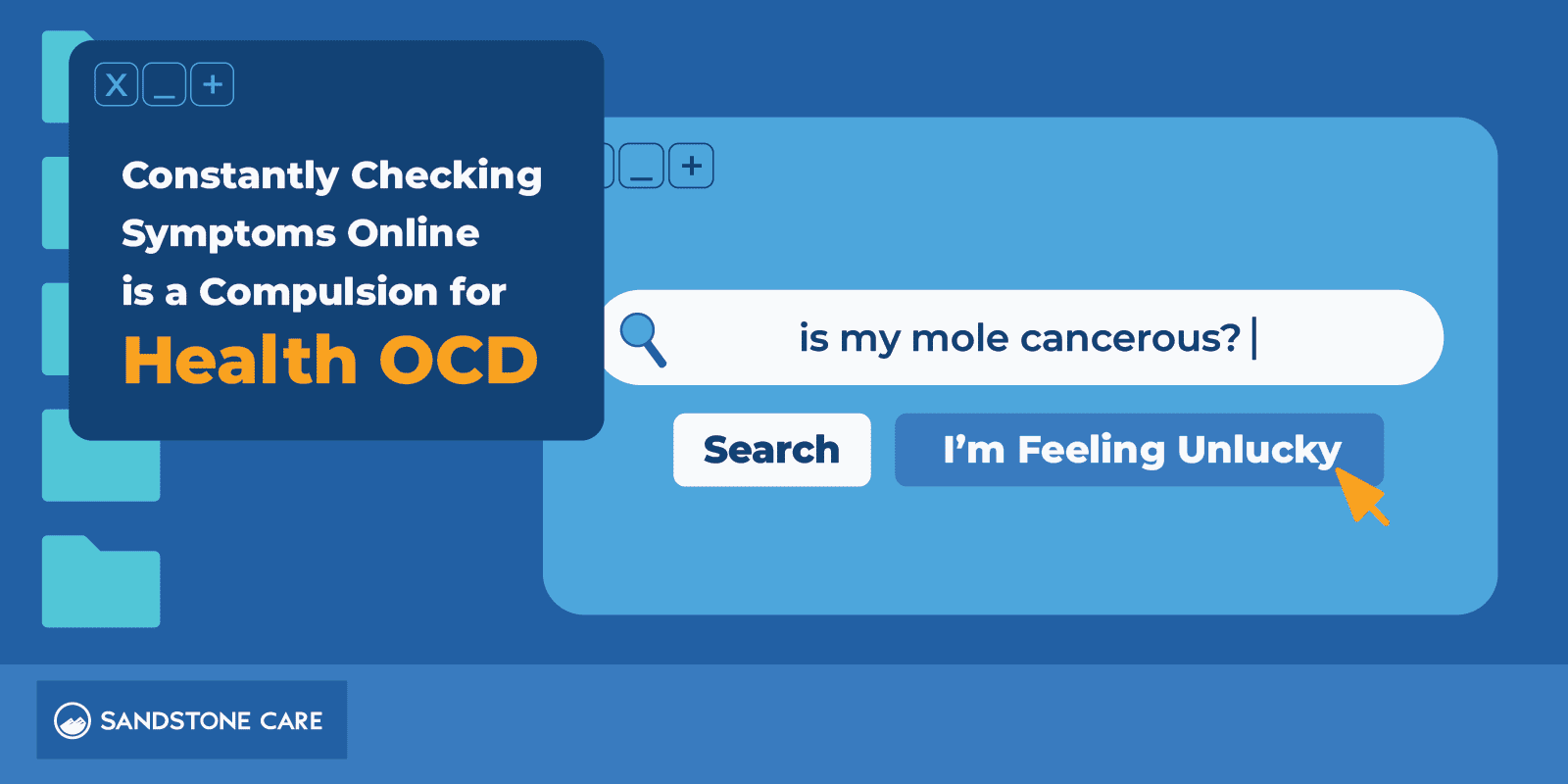
How Do You Manage Health OCD?
Health OCD may be managed by seeking help from a mental health treatment provider and receiving professional support and guidance in learning to manage your symptoms.
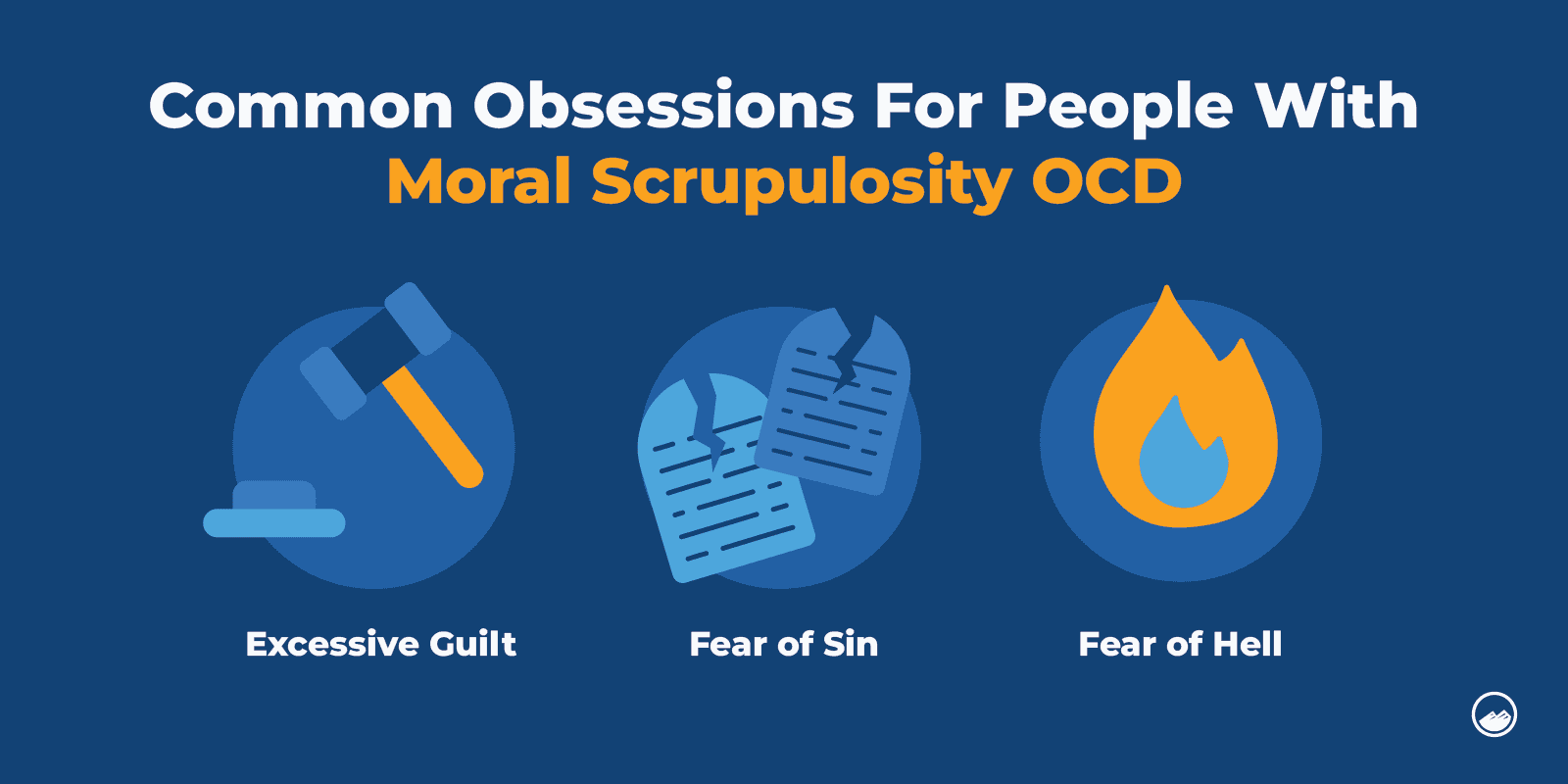
Moral or Scrupulosity OCD
What Is Scrupulosity OCD?
Scrupulosity OCD involves obsessions surrounding religion or morality.
- Obsessions: Concerns about morality, ethics, or religious correctness.
- Compulsions: Praying, seeking reassurance, or avoiding situations that trigger the obsessions.
What Are Moral Scrupulosity OCD Symptoms?
Moral Scrupulosity OCD involves obsessions and compulsions related to moral or ethical concerns.
Often, moral scrupulosity happens to people who are involved in religious communities. The specific symptoms of moral scrupulosity are different for everyone who experiences it, but if often reflects parts of the religious or moral structure they were raised in.
Some of the common obsessions associated with this type include:
- Excessive Guilt
Individuals with Moral Scrupulosity OCD often experience overwhelming guilt, even for minor or perceived moral transgressions. - Fear of Sin
There is an intense fear of committing a moral or religious sin. This fear is often strong enough that even when loved ones or religious leaders assure the sufferer that no sin has happened, they still feel uncertain. - Intrusive Religious or Moral Thoughts
People with scrupulosity struggle with consistent, distressing thoughts about religious or moral structures. For example, they may constantly feel that they are going to be condemned to hell if they do not pray in the exact right way.
Some of the common compulsions associated with scrupulosity include:
- Excessive Confessing
People with Scrupulosity OCD may feel an urge to confess what they believe are moral wrongdoings over and over again, seeking reassurance or forgiveness from others.
- Excessive Prayer or Rituals
People with scrupulosity might use rituals, like praying repeatedly or for excessive lengths of time, to try and feel less guilty or anxious. - Seeking Moral Certainty
People with Scrupulosity OCD often seek repeated reassurance from religious figures, authorities, or loved ones to make sure they haven’t done anything morally wrong.
- Avoidance Behaviors
People with Scrupulosity OCD may avoid harmless situations, people, or activities because they worry that these things might lead to moral problems, even when there’s no actual moral issue involved.
Is Scrupulosity OCD Curable?
While scrupulosity OCD does not have a complete cure, personalized treatment with cognitive behavioral therapy and exposure therapy helps people improve their lives and lower their symptoms.
It’s crucial to work closely with a mental health professional who specializes in OCD and Scrupulosity to create a personalized treatment plan tailored to the individual’s specific religious or moral concerns and challenges.
What Medication Is Used for Moral Scrupulosity OCD?
Selective Serotonin Reuptake Inhibitors (SSRIs) are an antidepressant medication most commonly used to treat OCD.
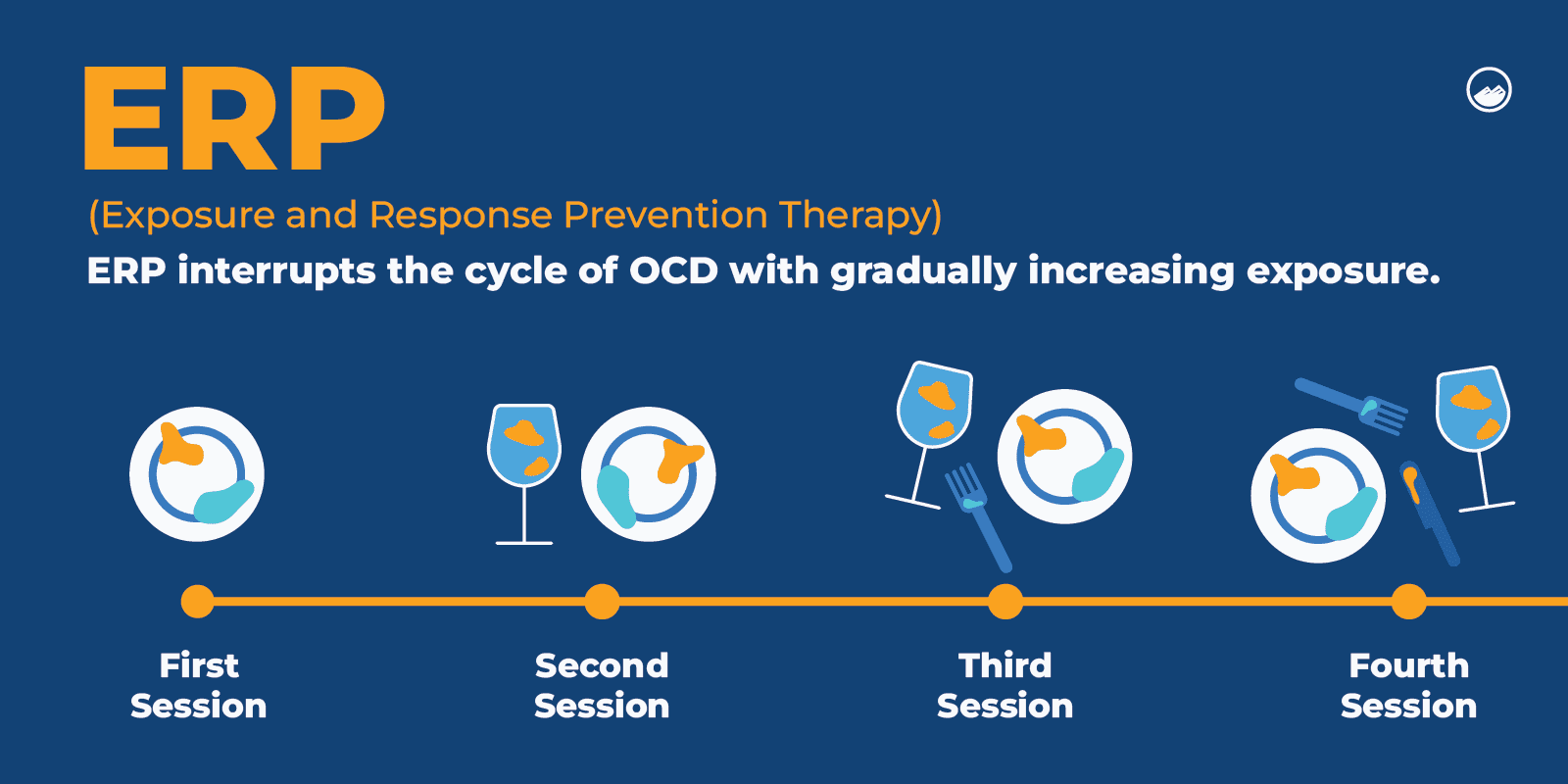
Treatment for OCD
What Are the Types of Therapy for OCD?
Cognitive behavioral therapy (CBT) is a common form of OCD treatment.
Exposure and response prevention therapy is a form of CBT that is common and effective in treating different forms of OCD.
Acceptance and commitment therapy (ACT) helps people with OCD by focusing on helping individuals accept their obsessions and uncomfortable thoughts without trying to control or eliminate them. Instead, it emphasizes committing to values-based actions and living a meaningful life despite the presence of obsessions.
Which Is the Best Therapy for OCD?
Exposure and response prevention therapy (ERP) is a common choice of therapy for various forms of OCD.
With ERP therapy, individuals are gradually exposed to their obsessions and learn how to not engage with their compulsions. By breaking the tie between their thoughts and actions, they are able to interrupt OCD’s cycle.
How Can I Cure My OCD Naturally?
OCD is not curable; however, outside of professional help, a person can do things such as managing stress, practicing mindfulness and meditation, exercising, and getting good rest to help manage the symptoms of OCD.
It’s also important to note that getting professional treatment for OCD doesn’t always involve medication. Talking to a therapist can help you find natural ways to improve your life, like changing your patterns of thinking and making sure you are getting the right amount of sleep for your brain.
FAQ
You Have Questions, We Have Answers.
Our goal is to provide the most helpful information. Please reach out to us if you have any additional questions. We are here to help in any way we can.
The four most common types of OCD include contamination OCD, harm OCD, symmetry or order OCD, and hoarding OCD.
Contamination OCD is characterized by an obsessive fear of becoming contaminated, especially with disease or illness.
The biggest variable in OCD treatment is unique to each person, so there is no specific type that is consistently more challenging than others.
However, types like purely obsessional OCD can be difficult to treat since there isn’t a compulsion to navigate.
OCD is a complex disorder, so treatment should be unique and personalized to each individual.
The cause of ROCD is unknown, but trauma may be a factor that contributes to the development of ROCD.

Let’s Take the Next Steps Together
OCD is a complex disorder that can manifest itself in many different ways. Learn more about the different types of OCD. Sandstone Care is here to support teens and young adults with mental health and substance use disorders.