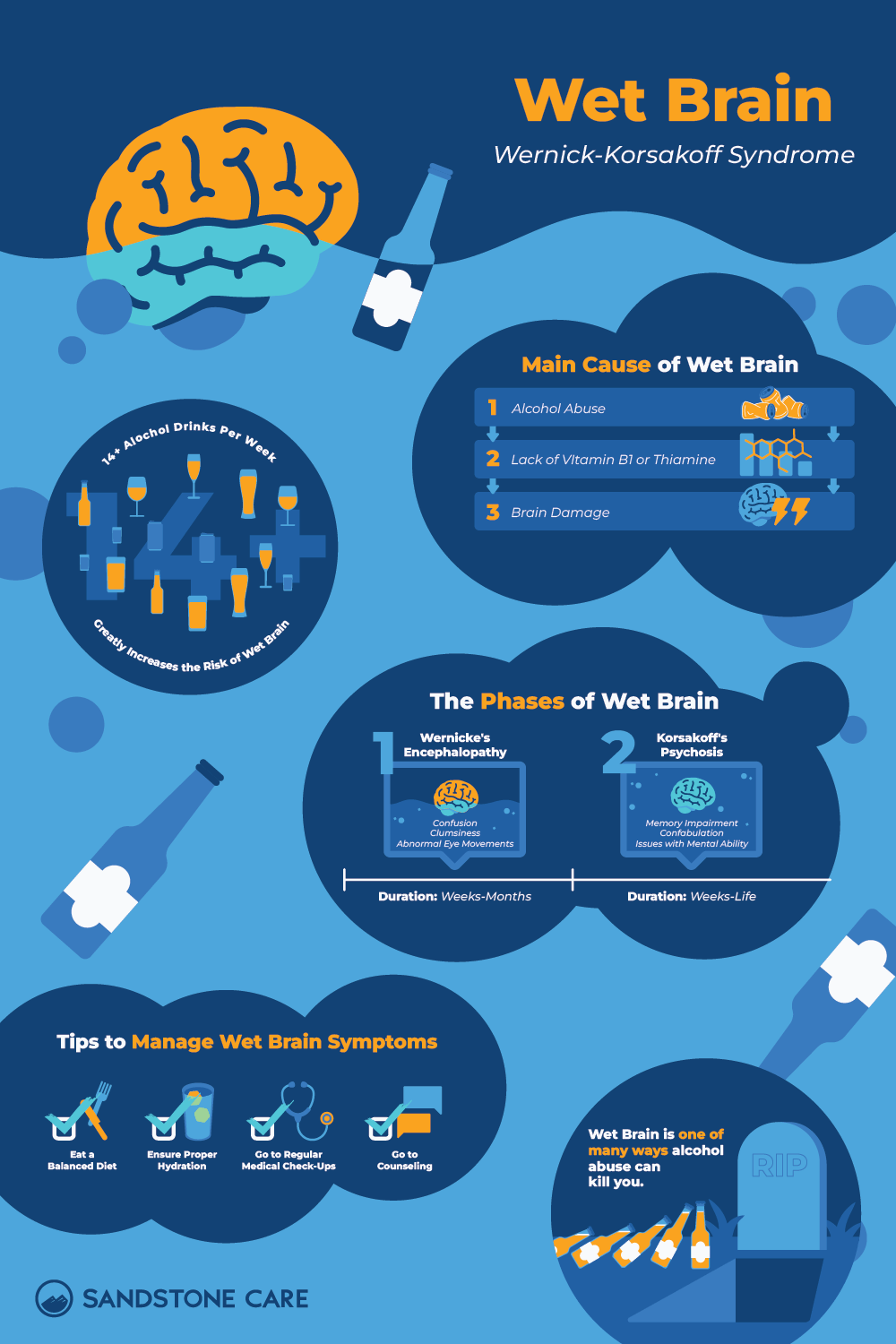
Wet Brain Syndrome
What Is Wet Brain?
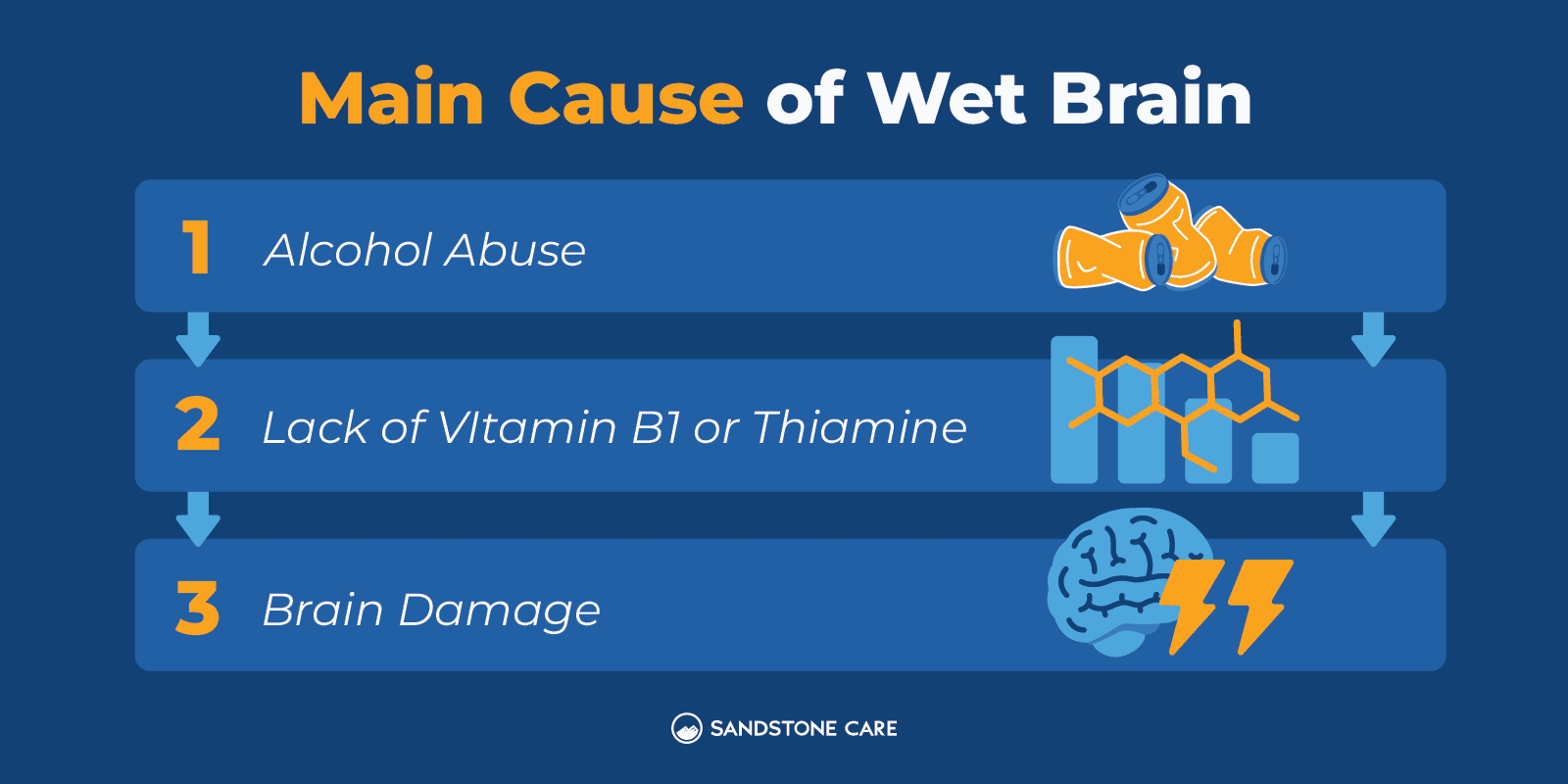
Wernicke-Korsakoff syndrome (WKS), sometimes called wet brain, is a brain disorder caused by a severe lack of vitamin B1 (thiamine). This condition happens in both short-term and long-term stages of the deficiency.
Lack of thiamine can occur due to long-term, heavy use of alcohol, dietary deficiencies, eating disorders, and chemotherapy. If left untreated it can cause serious physical impairments.
What Is the Medical Term for Wet Brain?
The medical term for wet brain is Wernicke-Korsakoff syndrome.
Wernicke-Korsakoff (WK) syndrome involves two brain disorders that most commonly occur together, which are Wernicke’s encephalopathy and Korsakoff’s psychosis.
Can Wet Brain Cause Dementia?
Yes, wet brain is a form of dementia caused by alcohol misuse and alcohol use disorder.
How Much Alcohol Causes Alcoholic Dementia?
According to recent studies, high-level alcohol consumption, which is considered to be more than 14 drink units per week, is associated with an increased risk of dementia.
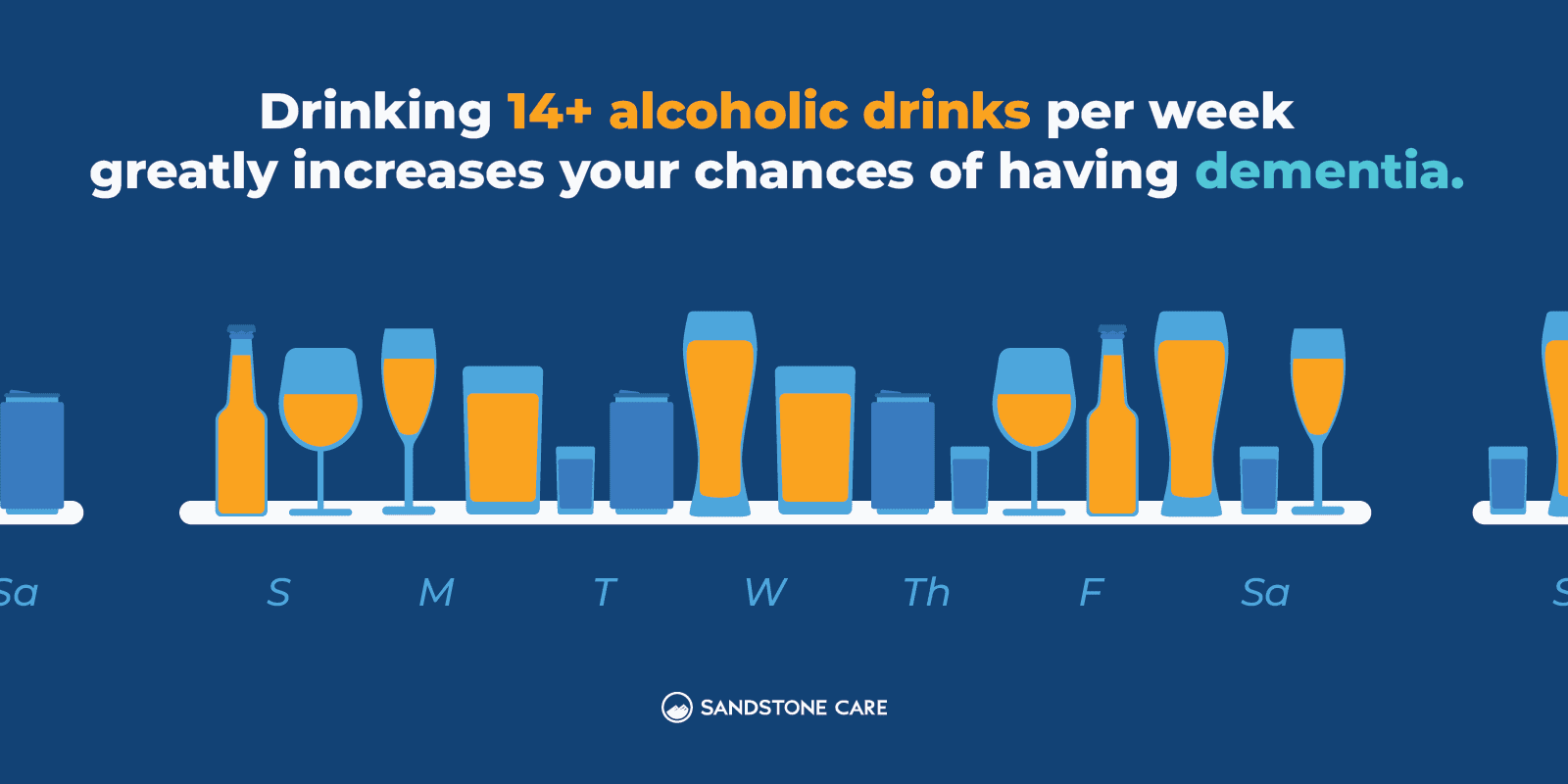
Other factors such as poor diet can also lower thiamine levels and lead to worsened symptoms. Maintaining a balanced diet can help individuals at risk of developing wet brain to start to get enough thiamine to lower their chances of alcoholic dementia.
However, the only way to fully avoid wet brain and alcoholic dementia is to lower the substance abuse itself.
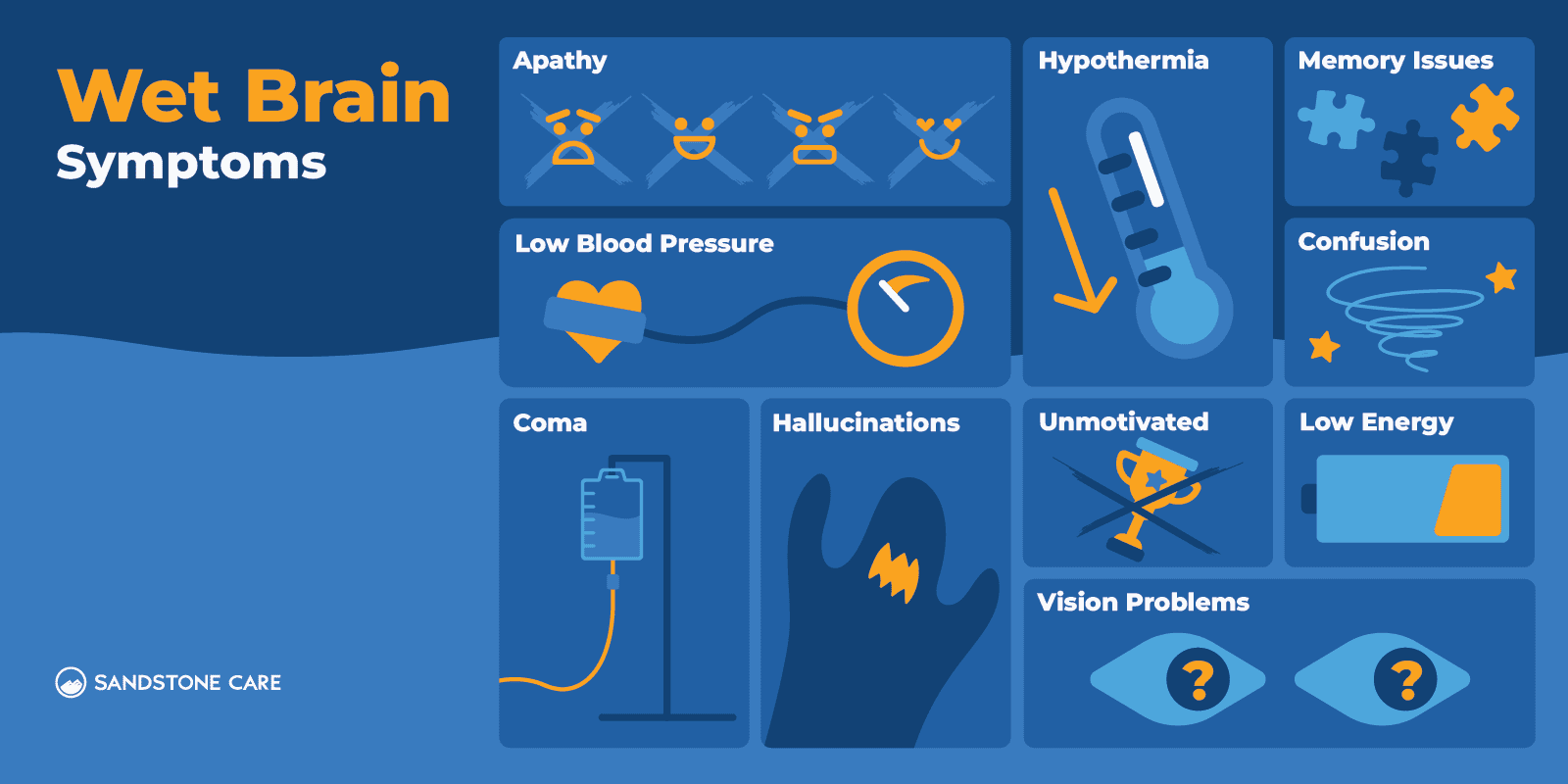
Wet Brain Symptoms
What Does Wet Brain Feel Like?
Wet brain can impact various brain regions including the thalamus, hippocampus, hypothalamus, and cerebellum. These regions play an important role in functions such as vision, movement, sleep, language, motivation, and memory.
A person with wet brain often feels confused and drowsy, along with many other physical symptoms that can include:
- Lack of energy
- Hypothermia
- Low blood pressure
- Coma
- Vision problems, such as double vision or drooping eyelids
- Abnormal eye movements
- Severe memory impairment, which can impact an individual’s ability to form new memories and can cause memory loss
- Hallucinations
- Trouble with decision-making, planning, organizing, or completing everyday tasks
- Lack of motivation
- Emotional apathy
What Is the Main Symptom of Korsakoff’s Syndrome?
The main symptoms of Korsakoff’s syndrome include confusion and memory problems.
What Are 5 Signs of Korsakoff’s Syndrome?
5 common signs and symptoms of Korsakoff’s syndrome can include:
- Loss of memory
- Making up stories, also known as confabulation
- Hallucinations
- Tremors
- Disorientation
What Does Wet Brain Look Like?
A person with wet brain syndrome often experiences memory loss and may become forgetful or seem confused and disoriented.
Individuals with wet brain may also appear poorly nourished and experience weakness and decreased coordination.

What Does Alcohol Dementia Look Like?
Alcohol abuse and alcohol addiction can be linked to various types of dementia including Alzheimer’s disease, Vascular Dementia, and Wernicke-Korsakoff syndrome.
Different types of dementia may have different signs and symptoms but can include:
- Memory loss
- Slowed speech
- Loss of muscle coordination
- Confusion
- Disorientation
- Impacted cognitive function
- Vision problems
- Malnutrition
Is Wet Brain a Disability?
Wet brain can cause permanent memory loss and impacted cognitive function that can lead to permanent disability.
What Is Confabulation in Wernicke-Korsakoff Syndrome?
Wet brain behavior can commonly involve confabulation.
Confabulation, sometimes called “honest lying,” is a neuropsychiatric disorder in which an individual creates a false memory without intending to be deceitful.
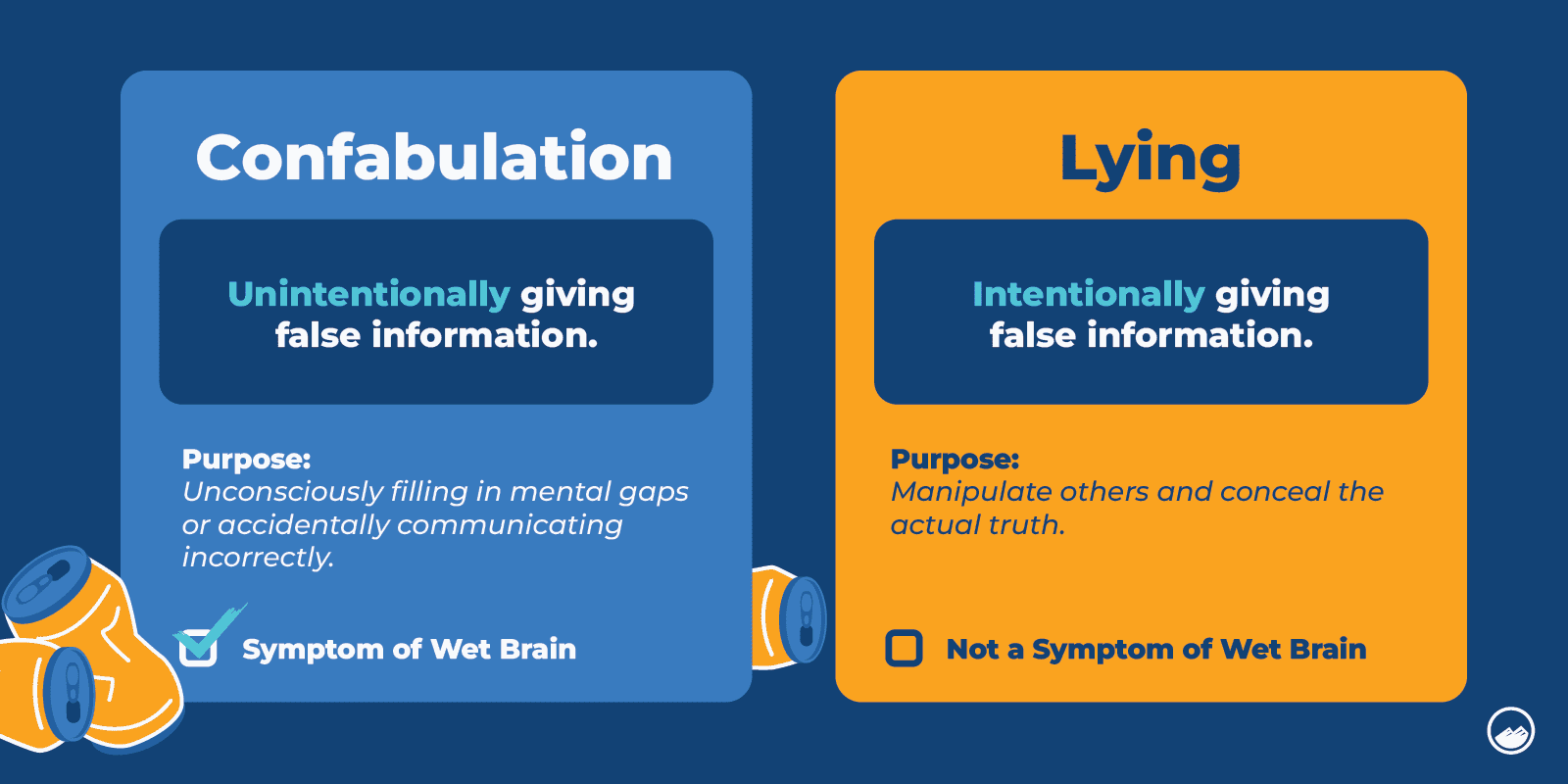
In Korsakoff’s syndrome, a person may have memories or recall experiences that never actually happened, however, they do not produce these false memories intentionally.
Individuals with memory loss may tell these lies as a subconscious way of filling in memories and details that they don’t remember.
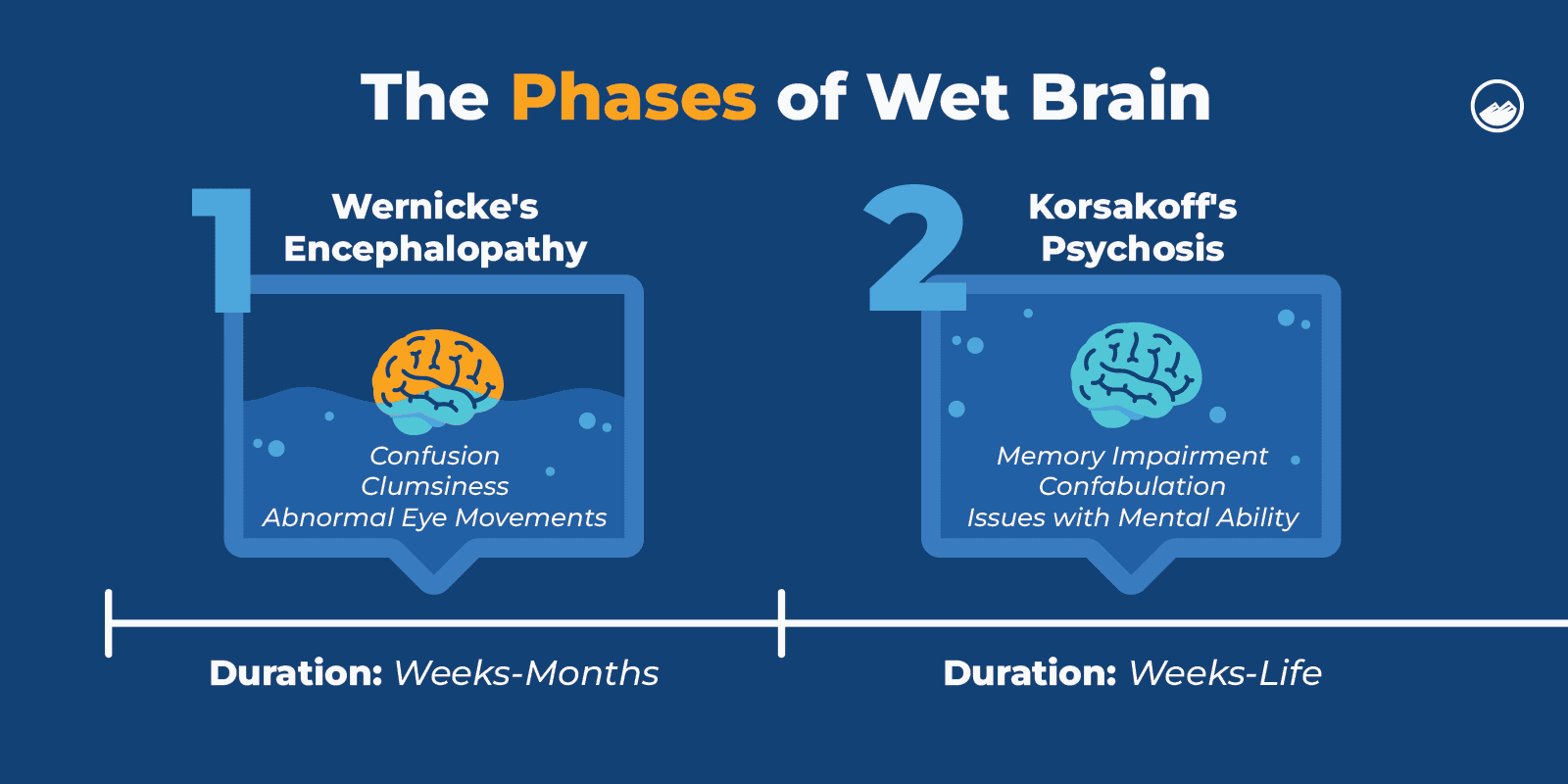
Wet Brain Stages
How Long Does It Take To Develop Wet Brain?
The symptoms of WK syndrome can take a few days to weeks to develop.
Wet brain typically develops in two separate stages. The first stage of wet brain is Wernicke’s encephalopathy, followed by Korsakoff’s psychosis.
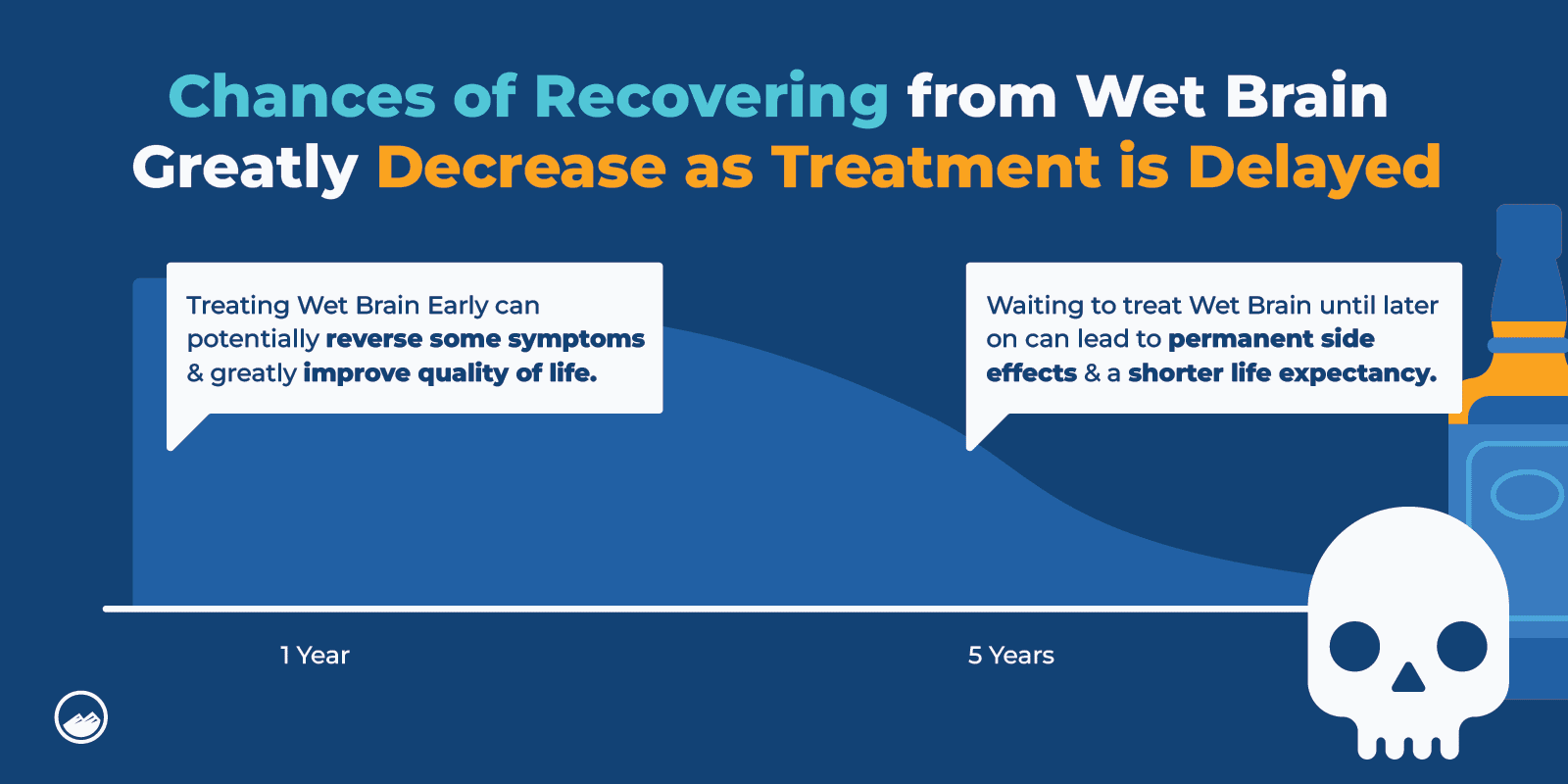
How Long Can You Live With Wet Brain?
Life expectancy for individuals living with wet brain can depend on a variety of different factors.
If caught early, some of the short-term effects caused by excessive alcohol use that lead to wet brain can be reversed and early detection can also help slow down the progression of this condition.
According to studies, the median survival estimate of individuals with alcohol-related Wernicke-Korsakoff syndrome was 8 years.
However, for individuals with other co-occurring disorders or health conditions related to alcohol abuse and who are in the later stages of alcoholism, the survival estimate can be much shorter and, in some cases, be as short as a few months.
If you have a loved one who may be showing symptoms of wet brain, it is crucial to reach out for help and consult with a professional to get a proper diagnosis and guidance on the steps you can take to get treatment.
What Are the Early Signs of Wet Brain?
The early stage of Wernicke-Korsakoff syndrome is Wernicke’s encephalopathy.
Common side effects and symptoms of Wernicke’s encephalopathy include mental confusion, loss of coordination, auditory hallucinations, apathy, and visual disturbances.
What Are the Early Signs of Alcohol Dementia?
Early signs of alcohol-related dementia can include:
- Memory loss
- Mood changes
- Personality changes
- Difficulty making choices
Does Wet Brain Come On Suddenly?
The symptoms of wet brain can come on suddenly, taking a few days to develop. While in others, it may take weeks and take longer to develop over time.
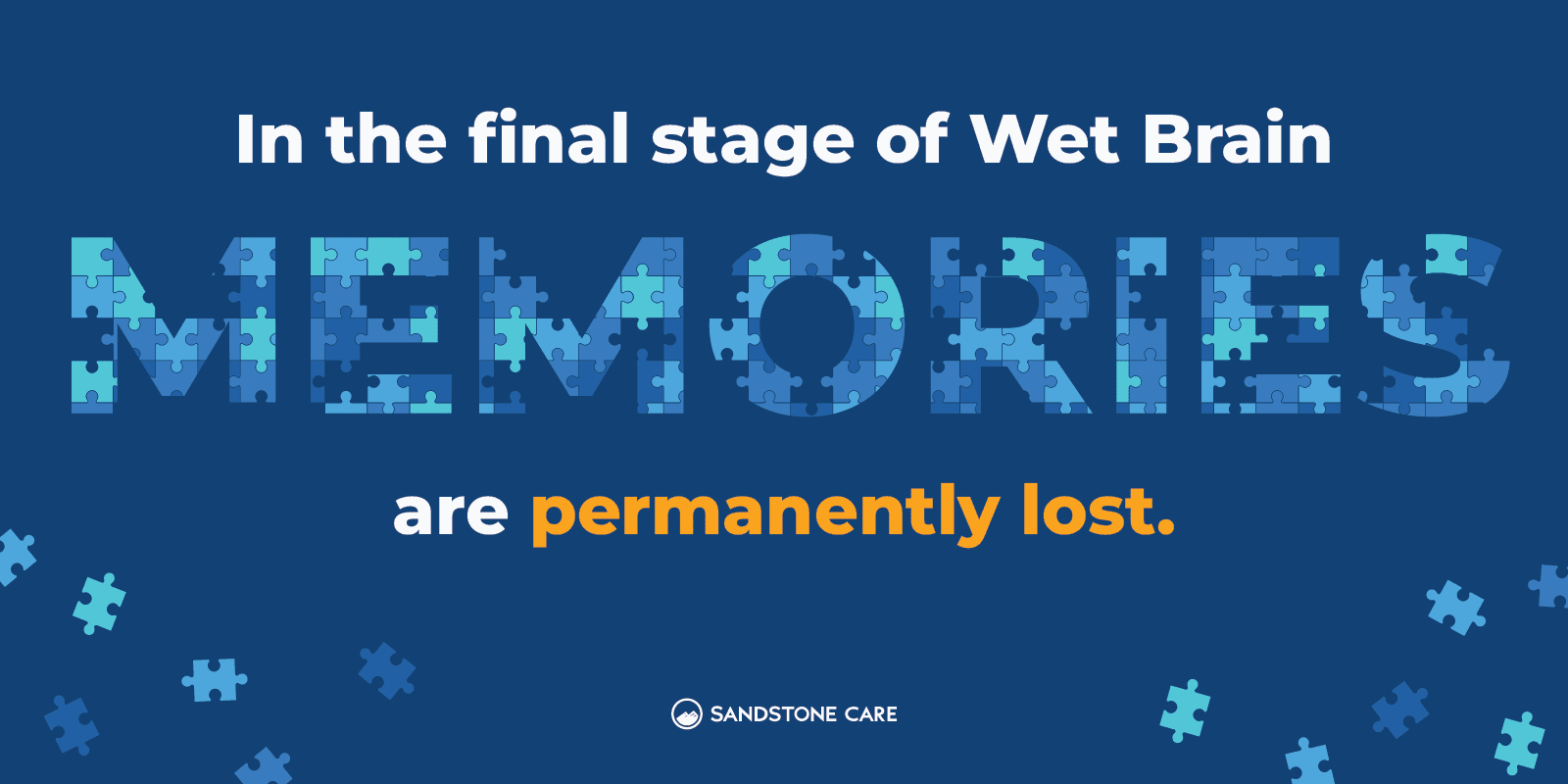
What Are the Final Stages of Wet Brain?
Often, when a person doesn’t receive treatment for wet brain, Wernicke’s disease can develop into Korsakoff’s psychosis.
In this stage, serious memory loss and other damage to the brain can become permanent.
In the final stages of wet brain, the ability to form new memories is often lost, and a person starts to progressively lose more memories. Unlike the early stages of wet brain, the effects in the final stages of wet brain are not reversible.
Wernicke-Korsakoff Syndrome Life Expectancy
Can Wet Brain Kill You?
Wet brain can cause severe symptoms and unfortunately in some cases, can result in coma or death.
This is one reason why it is important to catch the signs and symptoms of Wernicke-Korsakoff syndrome early to help keep some symptoms from worsening or developing over time and becoming more serious.
Wet brain deaths often result from Wernicke’s encephalopathy progressing and being left untreated.
How Serious Is Wet Brain?
Wet brain can progress and become a serious and in some cases, life-threatening disorder.
Excessive alcohol use and alcohol addiction can affect essentially every aspect of a person’s life. It can affect the brain, heart, liver, and pancreas, and put a person at a higher risk of certain cancers, according to the National Institute on Alcohol Abuse and Alcoholism.
Additionally, excessive alcohol use can cause mental health problems and affect a person’s everyday life, responsibilities, and relationships.
Alcohol addiction can lead to serious conditions, including wet brain which can be life-threatening if it progresses.

What Is the Life Expectancy of a Person With Wet Brain?
If a person is in the end stages of alcoholism, the life expectancy of a person with wet brain can be as little as six months.
However, early detection and proper treatment can help slow the progression of the disorder, even reverse some of the effects of excessive alcohol use, and help manage some of the symptoms of Wernicke-Korsakoff syndrome.
What Is the Usual Age Range of Korsakoff Syndrome?
The onset of wet brain symptoms typically starts between the ages of 30 and 70, and more commonly affects males than females.
Wet Brain Treatment
How Is Wet Brain Diagnosed?
If you have a loved one who may have wet brain, it is important to consult with a healthcare provider or a specialist such as a psychiatrist, addiction psychiatrist, or neurologist.
A doctor may do different exams to rule out any other conditions or possible causes, however, wet brain is most often linked to alcohol use disorder.
WK syndrome is diagnosed by looking at the individual’s history as well as the symptoms present.
If the presence of WK syndrome is suspected, they may confirm through a magnetic resonance imaging (MRI) scan.
Certain exams may be done to check the damage to the nervous or muscular system, as well as exams to check a person’s nutritional levels.
Early detection and proper diagnosis of Wernicke’s encephalopathy can allow for reversing some of the symptoms, which is why it is so important to reach out for help as soon as possible.
Is Wet Brain Commonly Diagnosed?
Researchers estimate that Wernicke-Korsakof syndrome is undiagnosed in about 80 percent of patients.
Wet brain is believed to occur in about 1 to 2 percent of the general population in the United States.
Individuals who chronically abuse alcohol are at a higher risk of developing wet brain.
How Is Wet Brain Treated?
Treatment for wet brain depends on the individual and what stage of wet brain they are in.
Doctors typically treat Wernicke’s disease with intravenous administration of vitamin B1, as well as glucose. Treatment for wet brain may also involve treating co-occurring conditions.
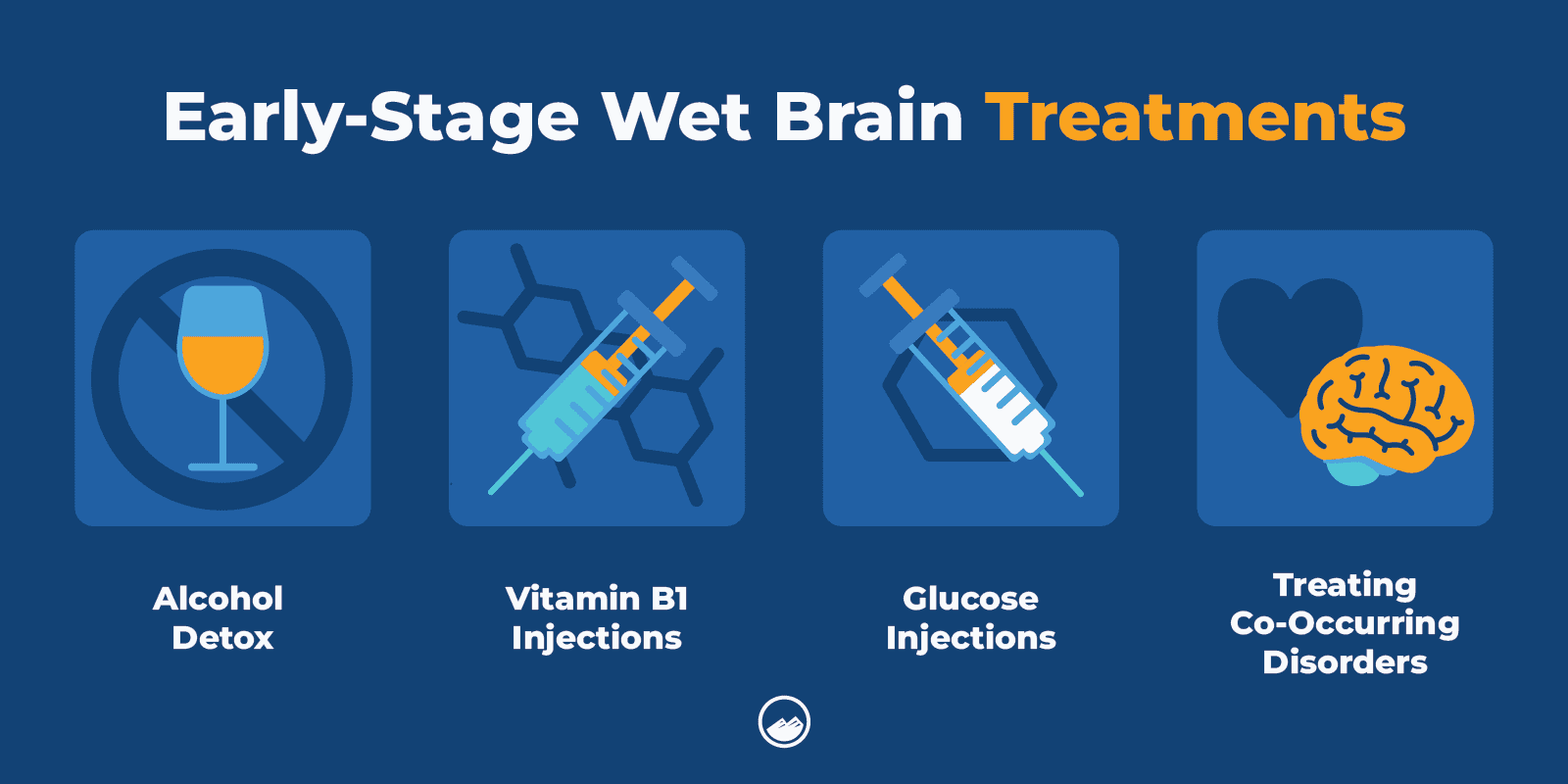
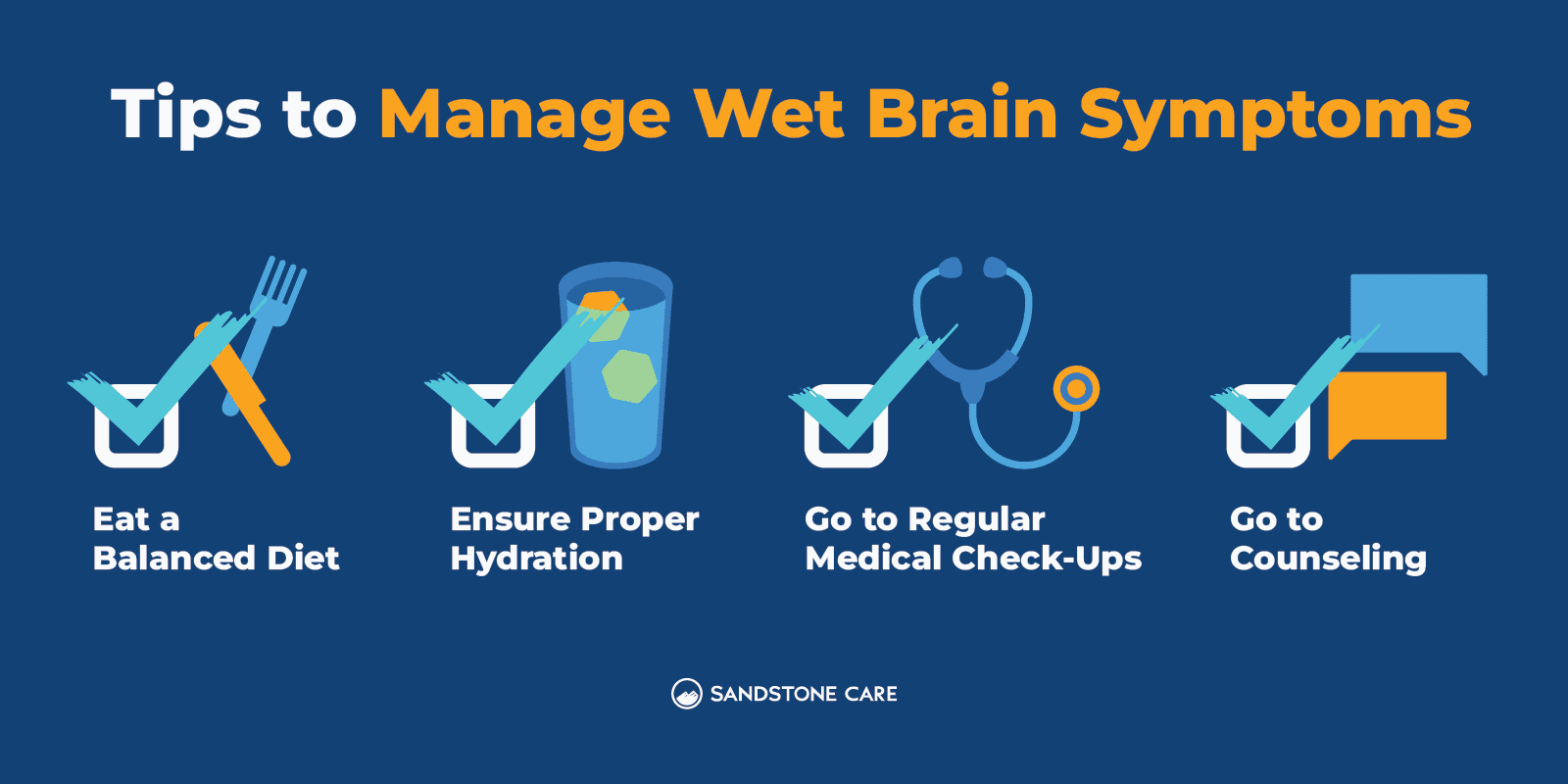
In the later stages of wet brain, if a person develops Korsakoff’s psychosis, treatment may include vitamin B1 replacement therapy, oral supplements, and making sure the individual gets proper nutrition and hydration.
It is important to remember that treatment for wet brain is not a one-size-fits-all. Treatment plans can depend on a variety of different factors such as the individual’s symptoms, the severity of their condition, and any other co-occurring conditions such as psychosis or other psychiatric disorders.
Some memory rehabilitation therapies, like ones used for other forms of dementia, can help a person manage their symptoms. However, for those with more severe cases, residential care is often needed.
Does Wet Brain Show Up on MRI?
Yes, research shows that wet brain can be seen on an MRI scan.
Studies show that Wernicke’s encephalopathy is most commonly seen on MRIs affecting the thalamus, mamillary bodies, periaqueductal and periventricular gray matter, and collicular bodies.
Can Wet Brain Be Cured?
Wet brain is not believed to be curable; however, with early detection and treatment, some of the effects may be reversible.
Treatment for wet brain can also slow down the rate at which this disorder progresses, helping individuals manage their symptoms and improve their quality of life. Receiving addiction treatment can seriously improve the future wellness of those who are at risk of developing wet brain from the effects of alcohol.
Is Wet Brain Reversible?
In the early stages of wet brain, Wernicke’s encephalopathy can be reversible with thiamine injections and ending the use of alcohol.
However, once a person is in the end stages of wet brain, or once it has developed into Korsakoff’s psychosis, the damage done to the brain is not reversible.
Permanent brain damage and other long-lasting neurological symptoms are consistently found in people with wet brain syndrome.
What Is the Goal of Wet Brain Treatment?
One of the most common goals of wet brain treatment is to manage symptoms and to help prevent the condition from worsening.
Sometimes, inpatient treatment options (including hospital stays) and special care is needed for individuals with wet brain if they are in a coma, lethargic, unconscious, or suffering from other medical conditions.
Will My Memory Improve if I Stop Drinking?
According to research, alcohol can have a serious impact on memory, specifically disrupting the ability to form long-term memories.
While these impacts can create lifelong damage to the brain and cognitive functions, individuals can find healing and improvements in cognitive functioning through recovery and quitting alcohol use.
Fortunately, the brain has an amazing ability to adapt and heal. However, the longer a person goes without getting help for alcohol use and continuing drinking over a long period of time, the higher the risk of severe damage may be.
While abstaining from alcohol is necessary in helping prevent or reduce more damage from Wernicke-Korsakoff syndrome, it is also important to keep in mind the symptoms of alcohol withdrawal.
Alcohol withdrawal can be extremely dangerous and in some cases, life-threatening. If you or a loved one are going through alcohol withdrawal, it is important to reach out for professional help to get the proper care and support you need.
A medical-assisted detox can help a person safely withdraw from alcohol with proper supervision, medication, and a safe environment.
What Are Alcohol Withdrawal Symptoms?
Alcohol withdrawal occurs when a person who has been drinking an excessive amount of alcohol regularly suddenly stops drinking.
Common symptoms of alcohol withdrawal can include:
- Anxiety or depression
- Fatigue
- Mood swings
- Not being able to think clearly
- Nausea and vomiting
- Rapid heart rate
- Tremors
In more severe cases, a person may also experience severe confusion, hallucinations, or seizures.
If you or a loved one are experiencing alcohol withdrawal symptoms, it is important to get professional help right away.
How Can You Prevent Wet Brain From Happening?
Abstaining from alcohol or drinking in moderation may help reduce the risk of developing wet brain, along with getting enough nutrition.
Thiamine supplements and a good diet can help individuals who face challenges with alcohol use. However, it will not eliminate the risk of the development of wet brain.
FAQ
You Have Questions, We Have Answers.
Our goal is to provide the most helpful information. Please reach out to us if you have any additional questions. We are here to help in any way we can.
Thiamine is an essential vitamin for the metabolism and function of brain cells.
Excessive alcohol use can contribute to a thiamine deficiency by impacting a person’s nutritional thiamine intake, decreasing the absorption of thiamine, and affecting the way thiamine is used in the cells, according to Alcohol Research and Health.
Supplementing with thiamine can help individuals who have an alcohol addiction reduce the risk of developing Wernicke’s syndrome and Korsakoff syndrome.
It is important to consult with your healthcare provider or another professional who can help you figure out the best and safest forms of treatment and therapy for alcohol use disorder and alcohol addiction.
Not all alcoholics get dementia, however, excessive alcohol consumption can impact the brain and may put a person at a higher risk of developing dementia.
Wernicke-Korsakoff syndrome is also sometimes referred to as alcohol dementia.
Alcohol-related dementia is diagnosed when alcohol abuse is most likely to be the cause of the symptoms of dementia a person is experiencing.
Alcohol dementia can impact a person’s memory, learning, reasoning, personality, mood, and social skills.
Alcohol can have a significant impact on the whole body, specifically the nervous system and the brain.
Excessive alcohol use can impact a person’s emotions and personality, and lead to impairments in perception, learning, and memory.
Some of the most common neurological conditions caused by alcohol can include dementia, polyneuropathy, and cerebellar degeneration. Fetal alcohol syndrome is also a condition that occurs due to alcohol exposure before birth.
A banana bag is a bag of fluids given intravenously to individuals for rehydration and vitamin and electrolyte deficiency.
Usually, a banana bag can contain folic acid, thiamine, and magnesium sulfate. The color of the solution is yellow, which is why it is often referred to as a banana bag.
Banana bags can help with nutritional deficiencies or imbalances in the body.
Individuals who describe their brain as feeling wet may be referring to Wernicke-Korsakoff syndrome, which is a brain disorder caused by thiamine deficiency and often related to long-term excessive alcohol use.

Let’s Take the Next Steps Together
Wernicke-Korsakoff syndrome, also commonly referred to as wet brain, is a serious brain disorder that can be life-threatening if not caught early and properly treated. Sandstone Care supports teens and young adults with mental health and substance use disorders.