Borderline Personality Disorder Overview
What Is Borderline Personality Disorder?
Borderline personality disorder, or “BPD,” is a mental health condition that makes it hard to regulate emotions and impulsivity.
People living with BPD often experience mood swings, negative self-image, and intense emotions that make it difficult to keep healthy relationships.
They may also show risky behaviors like reckless driving, binge eating, drug and alcohol use, unsafe sex, and self-harm.
While some people assume that those with BPD just lack self control, BPD is officially recognized by the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
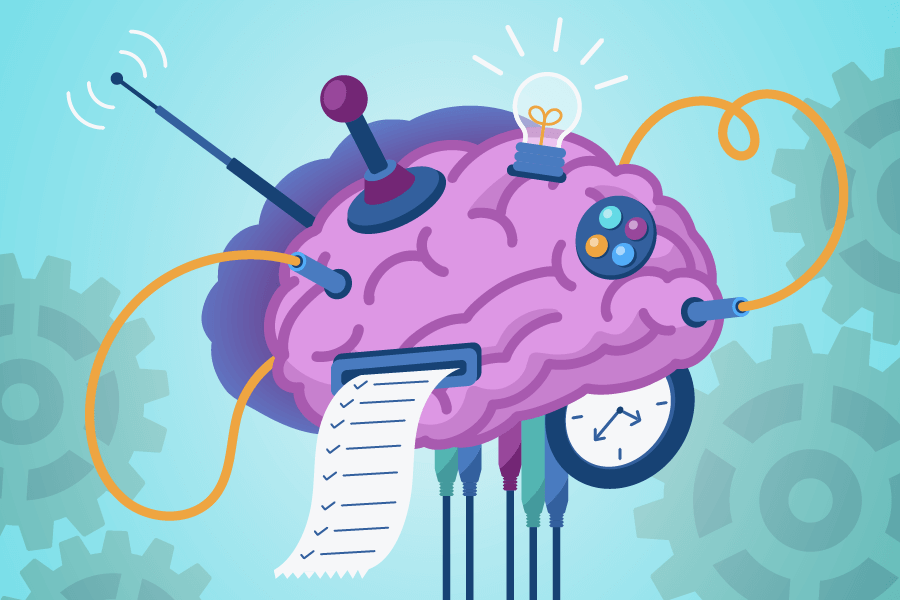
Borderline Personality Disorder (BPD) affects areas of the brain that control emotions and decision-making.
The amygdala is overactive in BPD, causing intense emotional reactions, even to minor situations.
At the same time, the prefrontal cortex, which helps with decision-making, is less active, making it harder for people with BPD to control impulsive behaviors.
Those with BPD also may have a hippocampus that does not work correctly, which can make it difficult for them to manage their stress in a healthy way.
Those living with BPD often describe living with the condition as if they seem to have “two different brains.”
The first brain is the real “them,” which is their identity.
The other is a chaotic force that drives them to disrupt their thoughts and actions.
This can make those struggling with BPD feel like they have no control over their lives.
Why Is It Called Borderline Personality Disorder?
Borderline Personality Disorder (BPD) got its name from older theories that said it was on the “borderline” between two types of mental health problems: neurosis (like anxiety) and psychosis (where someone loses touch with reality).
The term Borderline Personality Disorder (BPD) was first coined in 1938 by American psychiatrist Adolph Stern.
Stern observed patients who had severe emotional instability, but unlike those with psychosis (such as schizophrenia), they didn’t completely lose touch with reality.
Even though we now know BPD is its own, separate condition, the name has stayed the same over time.
What Does Borderline Personality Disorder Look Like?
Symptoms of Borderline Personality Disorder (BPD) may look like:
- Intense fear
- Paranoid thoughts
- Intense anger
- Mood swings
- Fear of abandonment
- Self-destructive thoughts
- Self-harming behaviors
- Risky, impulsive behavior
- Suicidal thoughts or suicide attempts
- Dissociation
Borderline Personality Disorder (BPD) can look different for everyone, but a common example is someone who experiences intense mood swings and fears of abandonment.
For instance, a person with BPD might have a close friendship where they feel connected one moment, but if the friend cancels plans, they may suddenly feel rejected and become very upset.
This could lead to impulsive actions, like sending desperate emotional messages or cutting off contact entirely. Impulsive symptoms can sometimes similar to histrionic personality disorder.
Struggling with emotional regulation because of BPD can lead to unstable relationships with loved ones and family members.
BPD may also look like sudden outbursts of anger towards loved ones.
As their relationships with others begin to fall apart because of these angry outbursts, people with BPD will often find themselves terrified of abandonment.
The paranoia of losing others can cause them to cling even more intensely to their relationships, leading to extreme emotional reactions.
Who Is Most Likely to Get BPD?
Those most at risk of getting BPD include:
- People who have gone through traumatic life events or post-traumatic stress disorder (PTSD)
- Those who come from toxic or unsafe home environments
- Victims of abuse, especially in childhood or early adulthood
- Those who are neglected emotionally and physically
It’s important to note that nobody is “immune” to developing BPD or any other mental illness, even if they do not have any obvious risk factors.
Is Borderline Personality Disorder Genetic?
Yes, genetics can play a role in Borderline Personality Disorder (BPD).
While there is no single “BPD-causing gene”, studies suggest that people with a family history of BPD may be more likely to develop the disorder.
BPD is also influenced by environmental factors, such as childhood trauma, abuse, or unstable relationships.
How Common Is Borderline Personality Disorder?
According to the National Institute of Mental Health, BPD affects about 0.7% to 2.7% of people.
While that may not sound very common, when you consider the size of the US population, those percentages are about the population of New York City.
BPD is more frequently diagnosed in women, but it is likely that men are under-diagnosed since they are less likely to seek medical treatment for their symptoms.
Is Borderline Personality Disorder the Same as Bipolar Disorder?
No, Borderline Personality Disorder (BPD) and Bipolar Disorder are not the same, though they share some symptoms like mood swings and emotional instability.
Borderline Personality Disorder and Bipolar Disorder affect different parts of the brain, but can sometimes overlap in what people experience.
It is also possible to be diagnosed with both BPD and bipolar disorder.
Some of the similarities between BPD and bipolar disorder include:
- Mood swings
Such as feeling abandoned after a minor disagreement. - Impulsivity
Such as overspending or unsafe sex. - Emotional instability
Such as intense, unpredictable emotional reactions. - Relationship difficulties
Such as frequent breakups or strained relationships.
Some of the differences between BPD and bipolar disorder include:
- Mood patterns
BPD has rapid mood shifts that can change within hours, while bipolar involves mood episodes lasting days or weeks. - Emotional triggers
BPD shifts are triggered by relationships or stress, while bipolar mood changes occur in manic and depressive phases. - Impulse control
BPD impulsivity happens almost constantly and is linked to emotional distress, while bipolar impulsivity mostly happens during manic episodes.
While BPD and bipolar disorder share some similar symptoms, they are unique conditions with different underlying causes and patterns.
This means that treatments that work for those with BPD may not work with those with bipolar disorder.
This why it is so crucial to have a mental health professional look closely at your health information and medical history to help find the best way to heal.
Signs of Borderline Personality Disorder
How Do I Know If I Have Borderline Personality Disorder?
If you experience intense emotions, fear of abandonment, unstable relationships, and impulsive behaviors, you may be showing signs of Borderline Personality Disorder (BPD).
Other symptoms include mood swings, feelings of emptiness, and trouble controlling anger.
Attempting to self-diagnose BPD is not recommended, and talking with a trained mental health professional is the only way to effectively and accurately determine if a person is living with BPD.
If you or a loved one are noticing potential signs or symptoms of BPD, calling local facilities like Sandstone Care can help each person further determine how BPD may be impacting their life.
What Does Untreated BPD Look Like?
Untreated Borderline Personality Disorder (BPD) often creates a repeating cycle of emotional reactions and impulsive actions that make the person feel intense mood swings and a constant fear of abandonment.
For example, when someone with Borderline Personality Disorder (BPD) feels abandoned, like when their partner doesn’t answer a phone call, they might assume they’re being ignored on purpose.
In the heat of the moment, they could send angry texts, accusing their partner of not caring or even threatening to end the relationship.
As emotions build, their brain’s amygdala, which processes intense emotions, goes into overdrive, making it hard to think rationally.
To escape the overwhelming feelings, they may engage in reckless behaviors like binge drinking or driving dangerously.
Afterwards, they often feel guilty and ashamed. That embarrassment and self-loathing can fuel their fears that they are unlovable.
This can restart the cycle of emotional outbursts, impulsive actions, and regret.
At What Age Does BPD Develop?
Borderline Personality Disorder (BPD) usually starts to develop in the late teens or early twenties.
Some early signs, like emotional swings, impulsive behavior, or relationship struggles, can show up in adolescence.
However, doctors often hold off on diagnosing BPD in younger people because teenagers are still going through normal emotional changes and personality development.
Waiting allows professionals to see if these patterns continue into adulthood before making a formal diagnosis.
Early support, though, can still be key to managing symptoms before they worsen.
Borderline Personality Disorder Splitting
What Is BPD Splitting?
BPD splitting a common symptom where someone with BPD begins to think of things in terms of extreme absolutes, effectively “splitting” everything into black-and-white.
This can cause an individual to catastrophize situations, overthink, compromise self-worth, experience unnecessary anxiety or fear of abandonment, and much more.
What Does a BPD Split Feel Like?
A BPD split can come with a lot of stress and conflicting emotions and can often feel as if a person’s “two brains” are battling it out to make sense of a certain stress or decision.
Rapid mood swings, stress, shifting between positivity and anger, and an inconsistent perception can make it feel impossible to make it through a split.
What Does a BPD Splitting Episode Look Like?
An individual experiencing a BPD split may rapidly change moods, think of things only in terms of absolutes, express intense fear or anger, or exhibit other forms of “all or nothing” thinking.
They may also rapidly shift between perspectives and opinions.
For example, those with BPD following a breakup may shift quickly between saying that they “never liked” their partner anyway, and then immediately follow it by sharing that they desperately loved and miss their partner.
What Triggers BPD Splitting?
Any perceived stress, difficult decision, or conflicting emotions and thoughts can trigger a BPD split.
Feelings of failure, perceived criticism, separations, or arguments can all cause a BPD-splitting episode.
Being reminded of certain people or places, especially if they are connected to past traumatic experiences, can also send someone into a BPD split.
How Long Do BPD Splits Last?
There is no definite time limit on BPD splits. Splits can last anywhere from a few hours to several days or even weeks.
A person may continue this way of thinking and reacting until the stresses are dealt with, or they find a better way to process the stresses or challenges they face.
Professional treatment and educated family members are important to help a person overcome a BPD split and improve daily quality of life.
Effects of Borderline Personality Disorder
BPD can have many effects on a person’s daily life and quality of life. In addition to compromised self-image and unstable relationships, BPD can also impact personal goals and responsibilities.
According to the American Psychiatric Association (APA), people with borderline personality disorder (BPD) often experience intense emotional pain and challenges in managing their relationships.
This emotional instability can lead to repeated crisis interventions or hospitalizations as they seek help for distressing symptoms.
Are People with Borderline Personality Disorder Dangerous?
No. People with Borderline Personality Disorder (BPD) are not inherently dangerous. While individuals with BPD may struggle with intense emotions, impulsivity, and self-destructive behaviors, this usually affects themselves more than others.
BPD can cause an individual to engage in angry outbursts and conflicts, but BPD on its own does not make someone a danger to those around them.
Can People with Borderline Personality Disorder Love?
Yes! While romantic relationships are often difficult to maintain for those living with BPD, they are absolutely capable of loving others.
Their emotional instability and fear of abandonment can make relationships challenging at times.
They may struggle with trust, shifting between idealizing and devaluing their partner, which can create emotional ups and downs in the relationship.
Despite these challenges, people with BPD are capable of forming strong emotional connections and caring deeply for others.
With the right support, such as therapy and emotional regulation skills, individuals with BPD can have healthy, loving relationships.
Borderline Personality Disorder Treatments
While BPD can greatly impact daily life, there are always treatment options available. Developing skills to manage the effects of BPD is always possible.
Given the nature of the illness, having a child or loved one with BPD can be extremely difficult and frustrating.
There can be a sense that the individual does not want to get better or is trying to manipulate you.
Symptoms tend to worsen without treatment and there are often periods of escalation during times of stress.
Getting experienced clinical treatment and realizing you are not alone is essential. There are available outpatient treatment centers that can help.
How Do You Get Diagnosed with Borderline Personality Disorder?
Talking to a trained mental health professional is the only way to receive an official diagnosis of BPD. Being open and honest in these discussions can be difficult but necessary to receive an accurate diagnosis and effective treatment.
How Is Borderline Personality Disorder Treated?
BPD is typically treated through a combination of talk therapy or psychotherapy, including cognitive-behavioral therapy (CBT,) dialectical behavior therapy (DBT,) dedicated problem-solving skills, suicide prevention, and more.
These strategies can also be combined to address other challenges, such as substance use disorder, anxiety disorders, and other challenges that happen alongside BPD.
What Is the Most Effective Treatment for Borderline Personality Disorder?
The most effective treatment for BPD is Dialectical Behavior Therapy (DBT), which is designed to help manage emotional ups and downs and impulsive behaviors.
DBT focuses on teaching skills that target specific challenges BPD individuals face:
- Mindfulness
Helps individuals stay focused on the present, which reduces overthinking about past or future worries. - Distress Tolerance
Teaches ways to cope with intense emotions without acting impulsively, preventing self-destructive behaviors like self-harm or substance use. - Emotion Regulation
Helps individuals recognize and manage strong emotions, making their mood swings less intense and easier to control. - Interpersonal Effectiveness
Teaches how to improve communication and set boundaries, which leads to healthier, more stable relationships without the fear of abandonment.
While other mental health services, like Cognitive Behavioral Therapy (CBT) or medications for anxiety and depression, can help, DBT is seen as the most effective approach for treating BPD symptoms.
While most treatments dialectical behavior therapy, to address the challenges of BPD, but there is no single treatment that is universally effective for everyone.
It is important, when seeking evidence-based psychiatry, to find a clinician that you feel comfortable with. If you are not able to open up about what is going on, then it is more difficult to make true progress.
Can Borderline Personality Disorder Be Cured?
BPD does not have a “cure” in the traditional sense. However, those living with BPD can develop the skills to manage its symptoms to improve their quality of life.
Does Borderline Personality Disorder Go Away?
BPD will not “go away,” and many of those living with BPD may continue to manage its effects throughout their life.
However, it is always possible to develop strategies to make BPD more manageable and create a fulfilling daily life with healthy relationships, positive feelings of self-worth, and more.
What Happens If BPD Is Left Untreated?
Left untreated, these “two brains” can continue to be at odds with each other, creating a tumultuous emotional state, unstable relationships, and possibly developing into other challenges.
Attempts to self-medicate untreated BPD with drugs or alcohol can develop into substance use disorder, while others may feel intense feelings of low self-worth that can lead to suicidal thoughts or even suicide attempts. Feelings of emptiness, abandonment, fear, and more can further these feelings.
This can also affect a person’s ability to hold a job or other responsibilities, affecting financial status and overall quality of life.
Borderline Personality Disorder Medication
Managing BPD is hard, but there are medication options available to help manage its symptoms.
Is There Medication for Borderline Personality Disorder?
Most commonly, antipsychotics are prescribed to help manage the effects of BPD. Others may use medications for anxiety disorders to help manage some of the symptoms of BPD.
There can also be an overlap in symptoms and challenges of BPD and ADHD, with some ADHD medications proving useful for managing certain symptoms of BPD.
What Is the Best Mood Stabilizer for Borderline Personality Disorder?
There is never a single medication that is best in all situations.
However, prescriptions for lithium are the most widespread mood stabilizer and have been effective in managing symptoms of BPD.